Conditions We Treat
We focus on patients and below is the conditions we treat

Low Back Pain
Back pain is an extremely common human phenomenon, a price mankind has to pay for their upright posture. Back pain can result from injury, activity, and some medical conditions. It can affect people of any age and for different reasons. As people get older, the likelihood of developing lower back pain increases Trusted Source due to factors such as previous occupation and degenerative disk disease.

Neck pain
Stiffness and pain in the neck usually result from overuse, injury, or sleeping in an unusual position. A stiff neck often occurs when one of the muscles becomes strained or tense. Stiffness can also develop if one or more of the vertebrae is injured. Neck pain is a common problem for IT profession. The common causes of neck pain are improper posture, Muscle strain, ligament sprain.

Knee pain
The knee joint is the most frequently injured joint. Osteoarthritis (OA) is a common chronic condition of the joints. It is a degenerative disease, caused by the “wear and tear” of the joints over time. We Bps Physiotherapy offers a best treatment protocol for neck pain with 100% results guarantee. We have advance tailor maid integrated approach with foreign practitioner Super specialist Physiotherapy

Carpal Tunnel Syndrome
Carpal tunnel syndrome is a common condition that causes numbness, tingling, and pain in the hand and forearm. It is caused by pressure on the median nerve. The median nerve runs from the forearm through a passageway in the wrist (carpal tunnel) to the hand. It provides sensation to the palm side of the thumb and fingers, except the little finger.
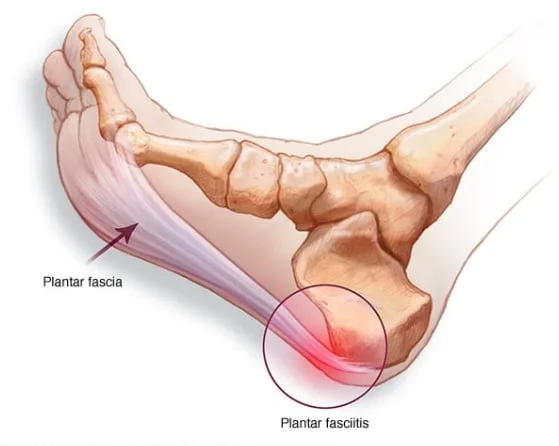
Plantar Fasciatis
Plantar fasciitis is inflammation in the plantar fascia in your foot. It’s the most common cause of heel pain. Plantar fasciitis commonly causes stabbing pain that often occurs with your first steps in the morning. As you get up and move, the pain normally decreases, but it might return after long periods of standing or when you stand up after sitting.
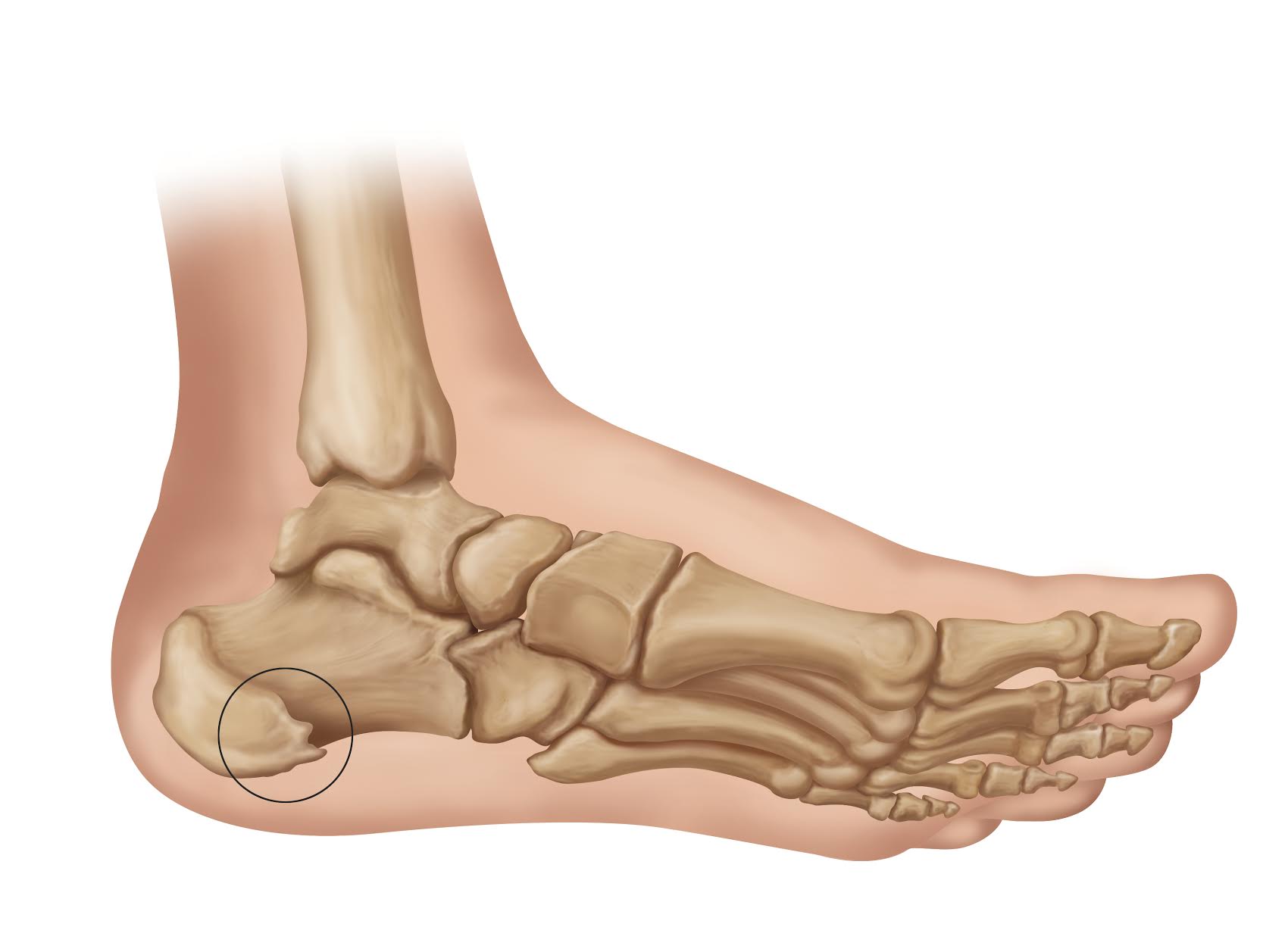
Calcaneus spur
Calcaneal spurs are bony growths at the back of the heel (dorsal) or under the sole of the foot (plantar). Calcaneus spurs occur when calcium deposits build up on the underside of the heel bone, a process that usually occurs over a period of many months. It’s too common on athletes whose activities include large amounts of running and jumping.

PCL Surgery
PCL same like ACL surgery. PCL surgery is the surgical repair of the posterior cruciate ligament (PCL) after a sprain, strain, or tear. PCL surgery is typically reconstructive surgery. During surgery, an orthopedic surgeon will remove the torn PCL and replace it with a tissue graft, either from your own body or from a deceased donor.

Cupping therapy
Cupping therapy is an ancient form of alternative medicine in which a therapist puts special cups on your skin for a few minutes to create suction. The practitioner will place cups on your skin. After that he will create a suction on your cups with help of a suction gun . You’ll feel a sucking sensation and pressure as the cups are suctioned.

Dry Needling
A specially trained physical therapist uses a thin needle to release muscle tightness, ease tendonitis and inflammation, and/or promote healing. During dry needling , a practitioner inserts several filiform needles into your skin. Filiform needles are fine, short, stainless steel needles that don’t inject fluid into the body.

Hijama
Hijama is the Arabic word for wet cupping, and refers to the process of raising the blood toward the skin and is then drawn by vacuum from a small skin incision for therapeutic purposes. Balances body to normal state: Cupping removes the toxins and stagnant fluids from your body through the blood sucked out.

Chiropractor
Chiropractic is the science and healing art of correcting and restoring joint mobility, thus reducing degenerative changes to joint surfaces, alleviating pain induced through nerve traction and compression. Patients often note positive changes in their symptoms immediately following treatment.

Physiotherapy
Physiotherapists help people affected by injury, illness or disability through movement and exercise, manual therapy, education and advice. They maintain health for people of all ages, helping patients to manage pain and prevent disease. Physiotherapy helps through physical rehabilitation, injury prevention, and health and fitness.
Conditions and Treatment Details
We care for your pain to recover very fast with worldclass treatments
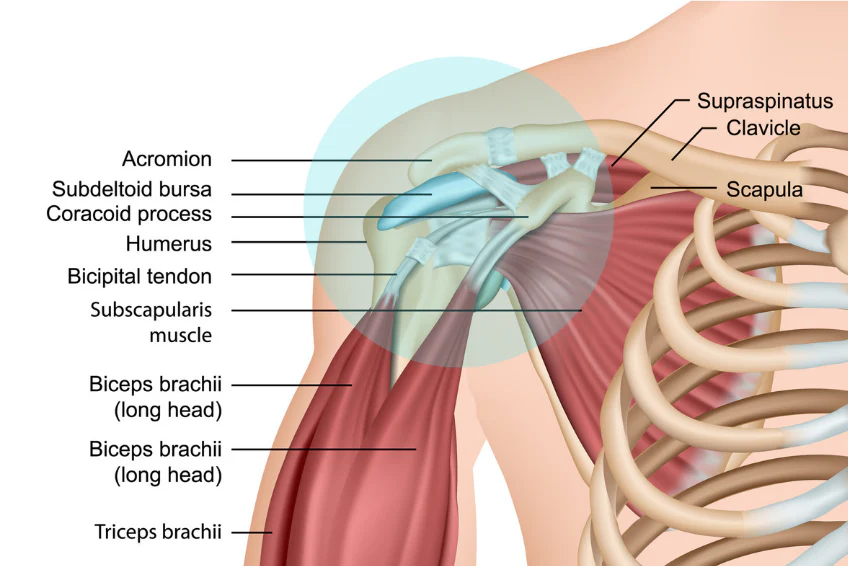
1. Shoulder pain

Introduction: Shoulder pain is a common ailment that can significantly impact daily life. It can arise from various causes and may be acute or chronic. Understanding the causes, symptoms, treatment options, and prevention strategies for shoulder pain is crucial for managing this condition effectively.
Causes:
• Muscle Strain: Overexertion or improper lifting can strain the shoulder muscles.
• Rotator Cuff Injuries: Tears or inflammation of the rotator cuff tendons.
• Frozen Shoulder: Characterized by stiffness and limited range of motion.
• Arthritis: Osteoarthritis and rheumatoid arthritis can affect the shoulder joint.
• Tendonitis: Inflammation of tendons in the shoulder, such as biceps or supraspinatus.
• Bursitis: Inflammation of the bursa sac in the shoulder.
• Fractures: Broken bones in the shoulder area.
• Referred Pain: Pain originating from the neck, heart, or other organs can radiate to the shoulder.
Symptoms:
• Pain: Dull, aching, or sharp pain in the shoulder.
• Stiffness: Difficulty moving the shoulder.
• Weakness: Reduced strength in the affected arm.
• Swelling: Inflammation around the shoulder joint.
• Cracking or Popping: Audible sounds during shoulder movement.
• Numbness or Tingling: May radiate down the arm.
• Limited Range of Motion: Difficulty raising or rotating the arm.
Treatment:
• Rest and Ice: Rest the shoulder and apply ice to reduce pain and inflammation.
• Physical Therapy: Exercises to improve strength and range of motion.
• Medications: Over-the-counter pain relievers or prescription drugs.
• Injections: Corticosteroids or hyaluronic acid injections.
• Surgery: For severe cases, including rotator cuff repair or joint replacement.
• Alternative Therapies: Acupuncture, chiropractic care, or massage.
Prevention:
• Proper Posture: Maintain good posture to reduce strain on the shoulders.
• Ergonomics: Adjust workstations and equipment for optimal shoulder comfort.
• Regular Exercise: Strengthen shoulder muscles and improve flexibility.
• Warm-Up and Stretch: Always warm up before physical activity.
• Lift Safely: Use proper lifting techniques to avoid strain.
• Avoid Overuse: Give the shoulder adequate rest between activities.
• Healthy Diet: Maintain a balanced diet to support joint health.
• Stay Hydrated: Proper hydration helps prevent muscle cramps and stiffness.
Shoulder pain can range from a minor inconvenience to a debilitating condition, and treatment should be tailored to its underlying cause and severity. Consulting a healthcare professional for an accurate diagnosis and personalized treatment plan is essential.
2. Ankle injury

Introduction: Ankle injuries are common and can range from minor sprains to more severe fractures. These injuries often result from various causes and can have a significant impact on mobility and quality of life. Understanding the causes, symptoms, treatment options, and prevention strategies for ankle injuries is crucial for effective management.
Causes:
• Sprains: Overstretching or tearing of ligaments due to sudden twisting or rolling of the ankle.
• Fractures: Broken bones in the ankle, including the tibia, fibula, or talus.
• Achilles Tendon Injuries: Inflammation or rupture of the Achilles tendon.
• Overuse: Repetitive stress on the ankle joint, common in athletes.
• Trips and Falls: Accidents that result in direct impact or twisting of the ankle.
• Repetitive Strain: Prolonged standing or walking, often in poor footwear.
• Chronic Conditions: Conditions like arthritis that affect the ankle joint.
Symptoms:
• Pain: Often severe, localized to the ankle.
• Swelling: Inflammation around the injured area.
• Bruising: Discoloration of the skin due to broken blood vessels.
• Instability: Difficulty bearing weight or maintaining balance.
• Stiffness: Limited range of motion in the ankle.
• Popping or Snapping Sensation: Indicative of ligament or tendon damage.
• Tenderness: Sensitivity to touch around the injured area.
Treatment:
• Rest: Allow the ankle to heal by reducing weight-bearing activities.
• Ice: Apply ice to reduce pain and swelling (20 minutes at a time, every 1-2 hours).
• Compression: Use a bandage or brace to support and stabilize the ankle.
• Elevation: Keep the ankle elevated above heart level to reduce swelling.
• Medications: Over-the-counter pain relievers (e.g.,ibuprofen) to manage pain and inflammation.
• Physical Therapy: Exercises to improve strength, flexibility, and range of motion.
• Casting or Splinting: For severe fractures or instability.
• Surgery: Sometimes necessary for severe fractures or tendon tears.
Prevention:
• Proper Footwear: Wear supportive shoes and avoid high heels or shoes with inadequate ankle support.
• Balance and Strength Training: Maintain ankle strength and stability through exercises.
• Warm-Up and Stretching: Always warm up before physical activities.
• Avoid Uneven Surfaces: Be cautious when walking or running on uneven terrain.
• Use Braces or Taping: If you have a history of ankle injuries, consider extra support.
• Know Your Limitations: Don't push your body beyond its capabilities during physical activities.
• Maintain a Healthy Weight: Excess weight can strain the ankle joints.
Ankle injuries should be promptly assessed by a healthcare professional, especially if the symptoms are severe or do not improve with self-care. Early and appropriate treatment is essential for a full recovery and to prevent long-term issues.
3. Wrist pain

Introduction:
Wrist pain is a common complaint that can arise from various causes and can significantly impact daily activities. Understanding the causes, symptoms, physiotherapy options, treatment approaches, and prevention strategies for wrist pain is important for effective management.
Causes:
• Repetitive Strain: Overuse of the wrist, common in activities such as typing or using handheld devices.
• Sprains: Stretching or tearing of ligaments, often due to falls or sudden impacts.
• Carpal Tunnel Syndrome: Compression of the median nerve in the wrist.
• Arthritis: Osteoarthritis or rheumatoid arthritis affecting the wrist joint.
• Fractures: Broken bones in the wrist, including the radius or ulna.
• Tendonitis: Inflammation of tendons in the wrist, like De Quervain's tenosynovitis.
• Ganglion Cysts: Non-cancerous lumps that can press on nerves.
• Nerve Compression: Compression of the nerves in the wrist, leading to pain and tingling.
Symptoms:
• Pain: Dull, sharp, or aching pain in the wrist.
• Swelling: Inflammation around the wrist joint.
• Stiffness: Difficulty moving the wrist, reduced range of motion.
• Weakness: Reduced grip strength and dexterity.
• Numbness or Tingling: Often radiating down the hand and fingers.
• Clicking or Popping Sensation: Indicative of joint or tendon issues.
• Instability: Feeling like the wrist might "give way."
Physiotherapy:
• Physical Assessment: A physiotherapist evaluates the wrist's condition and mobility.
• Pain Management: Techniques such as ice and electrotherapy to reduce pain and inflammation.
• Range of Motion Exercises: Exercises to improve wrist flexibility.
• Strengthening Exercises: Targeting the wrist and forearm muscles.
• Joint Mobilization: Manual techniques to improve joint function.
• Ergonomic Advice: Guidance on workspace setup and hand positioning.
• Bracing or Splinting: Use of supportive braces to protect and stabilize the wrist.
• Home Exercise Program: A tailored program to continue rehabilitation at home.
Treatment:
• Rest: Reducing activities that exacerbate the pain.
• Medications: Over-the-counter pain relievers or prescription drugs.
• Corticosteroid Injections: For severe inflammation.
• Surgery: For severe cases like fractures or carpal tunnel release.
• Occupational Therapy: To improve daily functioning for chronic conditions.
Prevention:
• Ergonomics: Maintain proper wrist alignment during work or activities.
• Frequent Breaks: Take regular breaks during repetitive tasks.
• Wrist Supports: Use wrist supports or ergonomic devices when needed.
• Strengthening Exercises: Incorporate wrist and forearm exercises into your routine.
• Stretching: Stretch wrist muscles and tendons regularly.
• Avoid Repetitive Strain: Alternate tasks to reduce wrist overuse.
• Healthy Lifestyle: Maintain a balanced diet and weight to reduce stress on joints.
Wrist pain can vary in severity and duration, and a healthcare professional can provide a proper diagnosis and recommend suitable treatment and preventive measures. Physiotherapy plays a valuable role in rehabilitation and pain management for many wrist conditions.
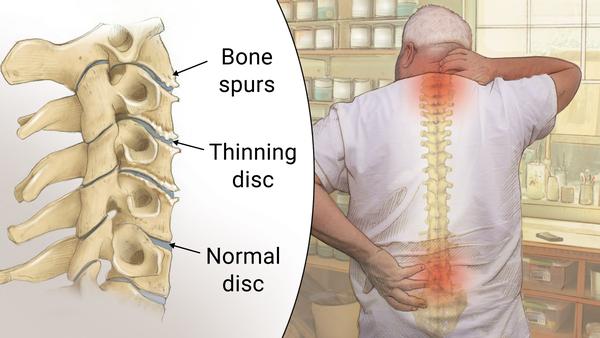
4. Spondylosis
Introduction:
Spondylosis is a degenerative condition that affects the spine, often associated with the aging process. It can occur in various regions of the spine, including the cervical (neck), thoracic (mid-back), and lumbar (lower back) areas.
Causes:
• Age-related wear and tear on spinal discs, leading to degeneration.
• Osteoarthritis, which affects the joints of the spine.
• Herniated or bulging discs.
• Bone spurs (osteophytes) that develop as a response to degeneration.
• Ligament thickening.
• Trauma or injuries to the spine.
• Poor posture and ergonomics over time.
Symptoms:
• Pain and Stiffness: In the affected area of the spine.
• Radiating Pain: Pain that may travel into the arms or legs, depending on the location of spondylosis.
• Numbness and Tingling: In the extremities.
• Weakness: Loss of muscle strength.
• Limited Range of Motion: Difficulty bending or turning.
• Neck or Back Pain: Chronic discomfort, which may worsen with movement.
• Headaches: In some cases, due to cervical spondylosis.
• Changes in Bowel/Bladder Control: In severe cases, for lumbar spondylosis.
Physiotherapy:
• Physical Assessment: Evaluation of the spine's condition and mobility.
• Pain Management: Utilization of techniques such as ice and heat therapy.
• Exercise Programs: Tailored exercises to improve spinal flexibility and strength.
• Manual Therapy: Hands-on techniques to alleviate pain and enhance mobility.
• Posture Correction: Education on maintaining proper posture.
• Ergonomic Advice: Guidance on creating ergonomic workspaces.
• Lifestyle Modifications: Recommendations for preventing exacerbation of symptoms.
Treatment:
• Medications: For pain relief and inflammation management.
• Physical Therapy: Physiotherapy programs as mentioned above.
• Supportive Devices: Braces or orthotics for spine support.
• Injections: Corticosteroid injections to reduce inflammation and pain.
• Surgery: In severe cases, such as spinal fusion or decompression.
Prevention: • Healthy Lifestyle: Maintain a balanced diet and manage weight.
• Exercise Regularly: Strengthen the muscles supporting the spine.
• Good Posture: Ensure proper posture when sitting and standing.
• Ergonomics: Create ergonomic work environments.
• Smoking Cessation: Smoking accelerates degeneration.
• Injury Prevention: Use proper techniques for lifting and bending.
5. Ankylosing Spondylitis
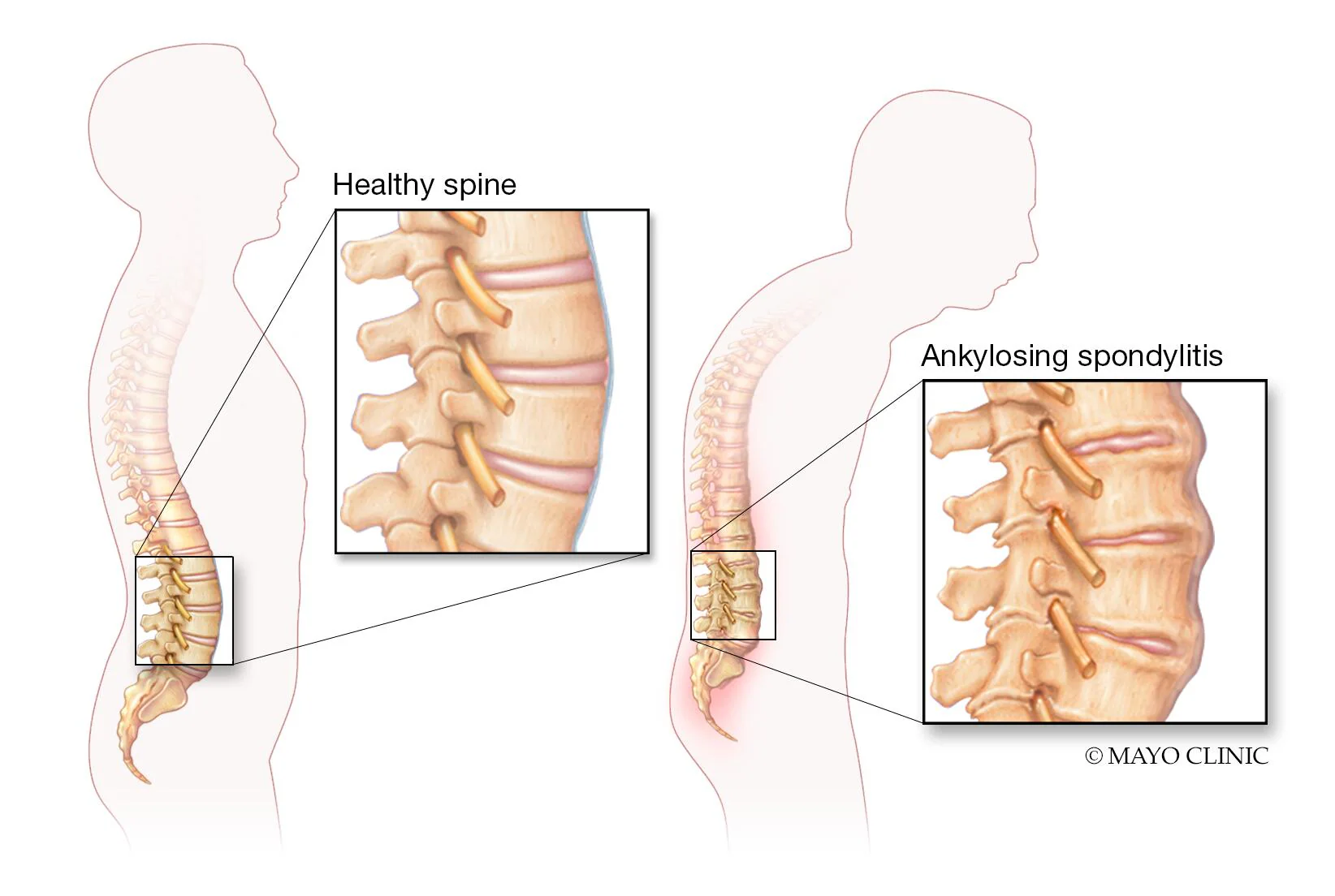
Ankylosing spondylitis (AS) is a chronic inflammatory condition that primarily affects the spine and sacroiliac joints. It is a type of spondyloarthritis, and here's a comprehensive overview:
Cause: The exact cause of ankylosing spondylitis is not known, but it is believed to have a strong genetic component, with the HLA-B27 gene playing a significant role. Environmental factors may also contribute to its development.
Symptoms:
• Back Pain: Persistent lower back pain and stiffness are common early symptoms.
• Spinal Fusion: Over time, AS can lead to the fusion of spinal vertebrae, causing reduced flexibility and posture changes.
• Pain in Other Joints: AS can affect other joints, like the hips, knees, and shoulders.
• Fatigue: Many people with AS experience fatigue.
• Eye Inflammation: Uveitis is an eye condition associated with AS.
Physiotherapy:
Physiotherapy is a crucial component of AS management. It can help improve flexibility, posture, and overall physical function. Exercises and stretches are tailored to the individual's needs to prevent or slow down the progression of spinal fusion.
Treatment:
• Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used to manage pain and inflammation. In more severe cases, biologics and disease-modifying antirheumatic drugs (DMARDs) may be prescribed.
• Physical Therapy: As mentioned, physiotherapy is essential for maintaining mobility.
• Exercise: Regular physical activity and specific exercises can help manage symptoms.
• Pain Management: Heat and cold therapy, as well as posture support, can alleviate pain.
• Surgery: In some severe cases, surgery may be necessary to correct deformities or replace damaged joints.
Prevention:
There is no known way to prevent ankylosing spondylitis, but early diagnosis and appropriate management can help control symptoms and prevent complications.
If you or someone you know is experiencing symptoms of AS, it's essential to consult a healthcare professional for a proper diagnosis and treatment plan.
6. Cauda equina syndrome
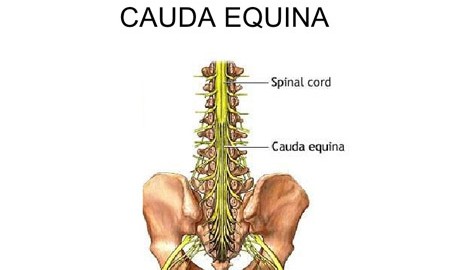
Cauda equina syndrome is a rare but serious medical condition that occurs when the bundle of nerves at the lower end of the spinal cord, known as the cauda equina, becomes compressed. Here's an overview of CES:
Cause:
CES is typically caused by a herniated disc, tumor, infection, spinal stenosis, or a severe injury. The compression of the cauda equina nerves can lead to various symptoms.
Symptoms:
• Lower Back Pain: Severe pain in the lower back is often a primary symptom.
• Leg Weakness: Weakness in one or both legs may occur, affecting mobility.
• Loss of Sensation: Numbness or tingling in the buttocks, genital area, or legs.
• Bowel and Bladder Dysfunction: Urgent or incomplete bladder and bowel control is a hallmark symptom.
• Sexual Dysfunction: Changes in sexual function can also occur.
Physiotherapy:
Physiotherapy can be an important part of CES rehabilitation, focusing on restoring strength, mobility, and coordination. It may help individuals regain function in their legs and pelvic muscles.
Treatment:
• Emergency Surgery: CES is a medical emergency, and prompt surgical intervention is often necessary to relieve the pressure on the nerves. This surgery aims to decompress the cauda equina and prevent permanent damage.
• Medications: Pain management and medications to address neurological symptoms may be used in conjunction with surgery.
• Rehabilitation: After surgery, physical therapy and rehabilitation may be needed to regain full function and mobility.
Prevention:
Preventing CES largely involves addressing underlying conditions that may lead to nerve compression, such as maintaining a healthy weight, proper lifting techniques, and seeking prompt medical attention for spinal issues.
It's crucial to recognize the symptoms of CES and seek immediate medical attention if you or someone you know experiences them, as timely treatment can significantly impact the outcome and prevent permanent neurological damage.
7. coccydnia
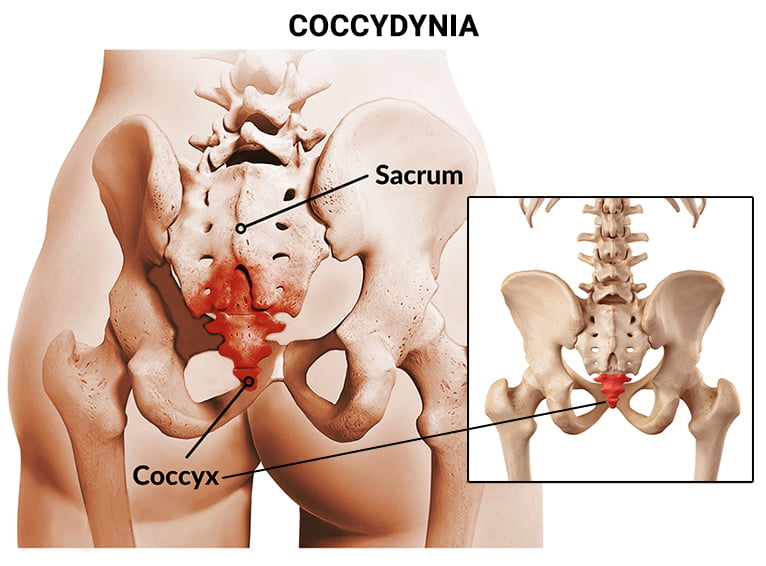
Coccydynia is a medical term referring to pain and discomfort in the coccyx, which is the small, triangular bone at the base of the spine, often referred to as the tailbone.
Cause:
Coccydynia can be caused by various factors, including trauma (such as falls or childbirth), repetitive strain, or in some cases, it may occur without a clear cause (idiopathic coccydynia).
Symptoms:
The primary symptom of coccydynia is pain and tenderness in the tailbone area. The pain may worsen when sitting, during activities that put pressure on the coccyx, or when transitioning from sitting to standing.
Physiotherapy:
Physiotherapy can be an effective treatment for coccydynia. It may include exercises to strengthen the pelvic floor muscles, improve posture, and reduce pain. Physiotherapists can also teach techniques for sitting and standing that reduce pressure on the coccyx.
Treatment:
• Conservative Measures: Rest, avoiding activities that exacerbate the pain, and using cushioning or donut-shaped pillows to relieve pressure while sitting.
• Medications: Pain relievers or anti-inflammatory medications may be prescribed.
• Physical Therapy: As mentioned, physiotherapy can be beneficial.
• Injections: In some cases, injections of corticosteroids may be used to reduce inflammation and pain.
• Surgery: Surgery is rarely considered and typically only when all other treatments have failed.
Prevention: Preventing coccydynia may involve avoiding situations that can lead to coccyx injury, using proper techniques when lifting heavy objects, and maintaining good posture.
If you're experiencing coccydynia, it's advisable to consult a healthcare professional for a proper diagnosis and to discuss appropriate treatment options.
8. Spinal Cord Injury
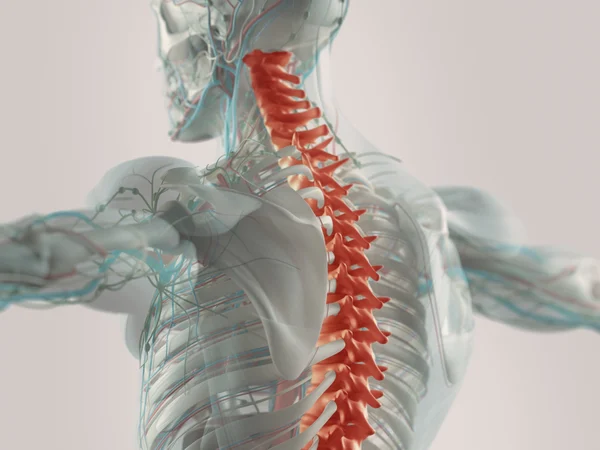
A spinal cord injury occurs when there is damage to the spinal cord, resulting in a loss of function or sensation below the level of the injury. Here's an overview:
Cause:
Spinal cord injuries can be caused by various factors, including traumatic incidents such as accidents, falls, sports injuries, or violence. Non-traumatic causes like tumors, infections, or degenerative diseases can also lead to SCI.
Symptoms:
The symptoms of a spinal cord injury depend on the level and severity of the injury. Common symptoms may include loss of sensation, muscle weakness or paralysis, changes in reflexes, loss of bowel or bladder control, and in severe cases, difficulty breathing.
Physiotherapy:
Physiotherapy, or physical therapy, is a critical component of the rehabilitation process for individuals with spinal cord injuries. It aims to maximize mobility, strengthen muscles, and improve overall physical function. Adaptive techniques and exercises are tailored to the individual's specific needs and capabilities.
Treatment: Treatment for spinal cord injuries is multi-faceted and depends on the nature and severity of the injury:
• Emergency Care: Immediate stabilization of the spine and medical attention to prevent further damage.
• Surgery: In some cases, surgery may be required to decompress the spinal cord or stabilize the spine.
• Rehabilitation: This includes physical therapy, occupational therapy, and speech therapy, among other forms of therapy, to regain lost functions.
• Medications: Medications may be prescribed to manage pain, muscle spasms, or other complications.
• Assistive Devices: The use of wheelchairs, orthotics, or other assistive devices can enhance mobility.
• Psychological Support: Coping with the psychological and emotional impact of an SCI is also a crucial aspect of treatment.
Prevention: Preventing spinal cord injuries involves safety measures such as wearing seatbelts in vehicles, using proper protective gear during sports, and taking precautions to prevent falls. Public education on safety measures can also help reduce the risk of spinal cord injuries.
The specific approach to treatment and rehabilitation will vary for each individual, depending on the location and severity of the spinal cord injury. Early intervention and a comprehensive care team are essential for optimizing outcomes in SCI cases.
9. Paralysis

Paralysis is the loss of muscle function in part or most of the body, often resulting from damage to the nervous system. Here's an overview:
Cause:
Paralysis can be caused by various factors, including:
• Stroke: A sudden interruption of blood flow to the brain can lead to paralysis, often on one side of the body.
• Spinal Cord Injury: Trauma or disease affecting the spinal cord can result in paralysis below the level of the injury.
• Neurological Conditions: Conditions like multiple sclerosis, cerebral palsy, and ALS can lead to paralysis.
• Traumatic Injuries: Falls, accidents, or other trauma can damage nerves or the brain, causing paralysis.
Symptoms:
The primary symptom of paralysis is the inability to move the affected muscles. Depending on the location and severity of the condition, it can impact a small region, a limb, or a substantial portion of the body. Paralysis may also affect sensory functions in the affected area.
Physiotherapy:
Physiotherapy plays a critical role in the management of paralysis. It focuses on maintaining or improving muscle strength, range of motion, and functional mobility. Techniques include exercises, stretching, and assisted movement to prevent muscle atrophy and improve quality of life.
Treatment:
• Underlying Cause: The treatment plan depends on the underlying cause of paralysis, and addressing this cause is a priority.
• Physical Therapy: As mentioned, physical therapy helps maintain or regain muscle function.
• Occupational Therapy: This focuses on developing skills for daily activities.
• Assistive Devices: Mobility aids, wheelchairs, and adaptive technologies can enhance independence.
• Medications: Medications may be prescribed to manage pain or address specific underlying conditions.
• Surgery: In some cases, surgical interventions may help alleviate pressure on nerves or repair damaged structures.
Prevention:
Preventing paralysis involves mitigating the risk of conditions or injuries that can lead to paralysis. This can include practicing safety measures, maintaining a healthy lifestyle to prevent stroke or neurological diseases, and using protective gear in high-risk activities.
The management of paralysis varies depending on the individual's condition, its cause, and its severity. A multi-disciplinary approach, involving healthcare professionals, physical therapists, and other specialists, is often necessary to provide the best care and support.
10. cerebral palsy

Cerebral palsy (CP) is a group of permanent movement disorders that appear in early childhood and affect a person's ability to control their muscles. Here's an overview:
Cause:
Cerebral palsy is primarily caused by damage to the developing brain, which can occur before birth, during birth, or in the first few years of life. The exact cause can vary and may include factors such as prenatal infections, brain injuries, genetic factors, or complications during birth.
Symptoms:
Symptoms of cerebral palsy can vary widely and may include:
• Difficulty with Movement: This can range from mild to severe, affecting one or more limbs.
• Spasticity: Increased muscle tone can lead to stiffness and reduced range of motion.
• Involuntary Movements: Some individuals with CP experience uncontrollable movements.
• Balance and Coordination Issues: Difficulty with balance and fine motor skills.
• Speech and Communication Challenges: Some may have difficulty speaking or communicating.
• Associated Conditions: CP can be accompanied by intellectual disabilities, seizures, or vision and hearing problems.
Physiotherapy:
Physiotherapy plays a crucial role in the management of cerebral palsy. It focuses on improving muscle strength, range of motion, and functional mobility. Exercises, stretches, and techniques are tailored to the individual to enhance their physical abilities and independence.
Treatment:
• Physical and Occupational Therapy: These therapies aim to improve motor skills and provide strategies for daily activities.
• Medications: Medications can help manage spasticity and other symptoms.
• Orthotic Devices: Braces or orthotics can assist with mobility and proper alignment.
• Speech and Language Therapy: For those with communication difficulties.
• Surgery: In some cases, surgical interventions may be needed to improve function or address complications.
Prevention:
Preventing cerebral palsy is not always possible, as the causes can be complex. However, prenatal care, avoiding maternal infections, and taking measures to prevent head injuries in infants can reduce the risk.
Early diagnosis and intervention are crucial for individuals with cerebral palsy. A comprehensive, multidisciplinary approach involving healthcare professionals, therapists, and educators can help improve the quality of life and functional abilities for those with CP.
11. Cervical disc buldge
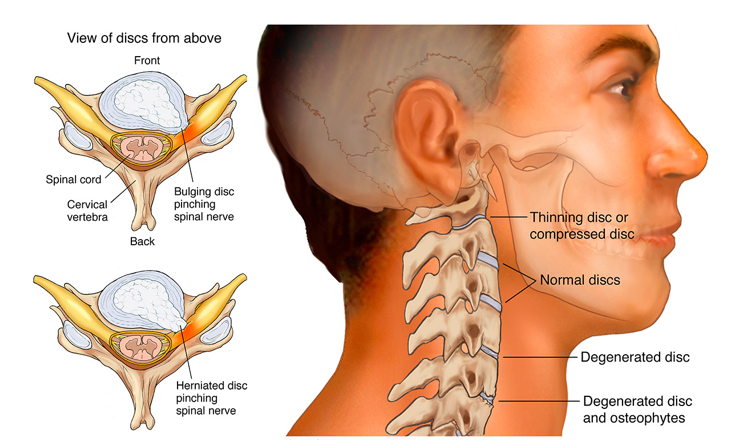
A cervical disc bulge is a condition where one of the discs in the neck (cervical spine) protrudes or bulges outward, often due to wear and tear. Here's an overview of its causes, symptoms, physiotherapy treatment, and prevention:
Causes:
• Aging: Disc degeneration is a natural part of aging and can lead to bulging discs.
• Injury: Trauma or accidents can damage cervical discs.
• Poor Posture: Maintaining incorrect posture over time can stress the cervical spine.
• Genetics: A family history of spine issues can increase the risk.
• Repetitive Motion: Certain occupations or activities that involve repetitive neck movement can contribute.
Symptoms:
• Neck Pain: Pain in the neck region is a common symptom.
• Radiating Pain: Pain may extend into the arms or shoulders.
• Numbness and Tingling: Sensations of numbness or tingling in the arms or hands.
• Weakness: Muscle weakness, particularly in the upper limbs.
• Stiffness: Reduced neck mobility and stiffness.
Physiotherapy Treatment:
• Physical Therapy: A physiotherapist can create a customized exercise and stretching plan to improve neck strength and flexibility.
• Manual Therapy: Hands-on techniques to reduce pain and improve mobility.
• Posture Education: Learning proper posture to prevent further stress on the neck.
• Ergonomic Adjustments: Modifying workstations and daily activities to reduce strain.
• Pain Management: Techniques like heat or cold therapy to alleviate pain.
Prevention:
• Maintain Good Posture: Be mindful of your posture, especially during extended periods of sitting or computer use.
• Stay Active: Regular exercise to strengthen neck and back muscles can help support the spine.
• Ergonomics: Ensure your workspace is ergonomically designed.
• Lift Properly: When lifting heavy objects, use your legs and not your back.
• Avoid Smoking: Smoking can accelerate disc degeneration.
It's essential to consult a healthcare professional for a proper diagnosis and treatment plan if you suspect a cervical disc bulge.
12. Lumbar disc buldge
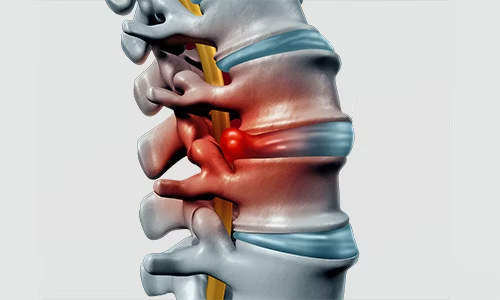
A lumbar disc bulge, also known as a herniated disc or slipped disc, is a common spinal condition that can cause back and leg pain. Here's an overview of its introduction, causes, symptoms, physiotherapy treatment, and prevention:
Introduction:
• A lumbar disc bulge occurs when one of the discs in the lower back (lumbar region) protrudes or bulges out of its normal position.
• This can put pressure on nearby nerves, leading to various symptoms.
Causes:
• The primary cause is the aging process, which results in disc degeneration and weakening.
• Other factors, such as poor posture, repetitive lifting, or traumatic injury, can contribute to disc bulges.
Symptoms:
• Symptoms may include lower back pain, sciatica (radiating leg pain), numbness, tingling, or weakness in the legs.
• Pain may worsen with certain movements or positions.
Physiotherapy Treatment:
• Physiotherapy can be an effective treatment option for lumbar disc bulges.
• Treatment typically involves:
• Pain management techniques like ice or heat therapy.
• Gentle exercises to improve flexibility and strength.
• Postural education to reduce strain on the spine.
• Manual therapy to alleviate pain and restore mobility.
• Core stabilization exercises to support the spine.
• Gradual progression of activities to prevent re-injury.
Prevention:
• Maintain good posture when sitting, standing, and lifting objects.
• Engage in regular exercise to strengthen the core and back muscles.
• Avoid excessive sitting and incorporate breaks to move around during the day.
• Practice proper body mechanics when lifting heavy objects.
• Maintain a healthy weight to reduce stress on the spine.
It's important to consult with a healthcare professional or physiotherapist for an accurate diagnosis and personalized treatment plan if you suspect a lumbar disc bulge.
13. Spinal canal stenosis
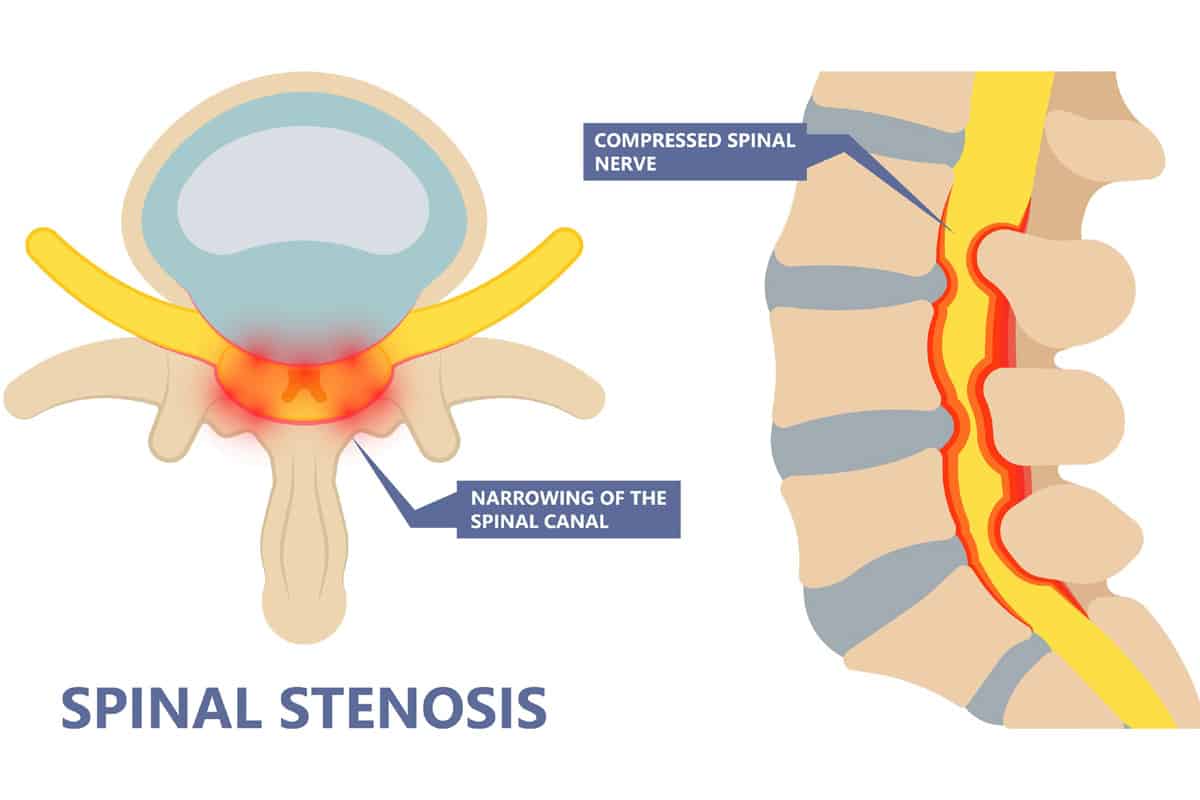
Spinal canal stenosis is a medical condition characterized by the narrowing of the spinal canal, which can put pressure on the spinal cord and nerves.
Spinal canal stenosis is a condition where the spinal canal, a passageway for the spinal cord and nerves, becomes narrowed, often due to degenerative changes.
This narrowing can lead to compression of spinal structures, resulting in various symptoms.
Causes:
• Aging is a common cause, as it leads to degenerative changes in the spine, such as the development of bone spurs or thickening of ligaments.
• Other causes can include herniated discs, spinal injuries, congenital conditions, and inflammatory disorders.
Symptoms:
• Symptoms may include pain, numbness, tingling, and weakness in the back, legs, or arms.
• Pain can worsen when standing or walking, and it may be relieved when sitting or bending forward.
• Some individuals experience difficulty with balance and coordination.
Physiotherapy Treatment:
• Physiotherapy can be beneficial in managing spinal canal stenosis. Treatment aims to improve function and alleviate symptoms.
• Components of physiotherapy may include:
• Stretching and flexibility exercises to reduce muscle tension.
• Strengthening exercises to support the spine and improve posture.
• Balance and coordination exercises.
• Pain management techniques, such as heat or ice therapy.
• Postural education and ergonomics to minimize stress on the spine.
Prevention:
• There are steps you can take to help prevent or slow the progression of spinal canal stenosis:
• Maintain a healthy weight to reduce strain on the spine.
• Engage in regular physical activity to keep the spine flexible and strong.
• Use proper body mechanics when lifting heavy objects.
• Consider lifestyle modifications, such as avoiding prolonged standing or walking if you have risk factors.
If you suspect spinal canal stenosis, it's essential to consult with a healthcare professional for a proper diagnosis and to discuss the most appropriate treatment and management options for your specific condition.
14. Spondylolisthesis
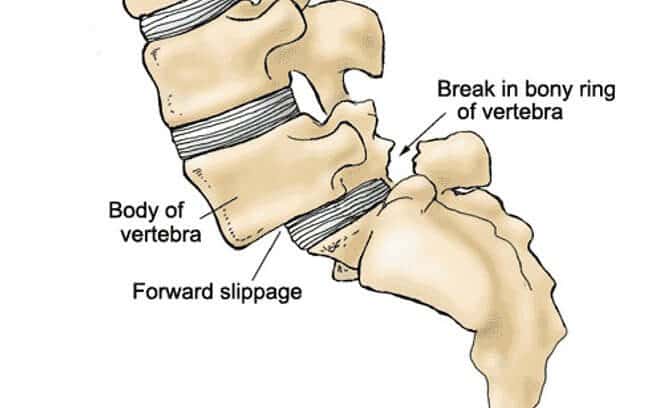
Spondylolisthesis is a spinal condition in which one vertebra slips forward over an adjacent vertebra, typically in the lumbar (lower back) region.Spondylolisthesis is a condition that occurs when one vertebra, often in the lumbar spine, shifts out of its normal position and moves forward or backward relative to the adjacent vertebra. This condition can result from a variety of causes and can lead to symptoms and complications.
Causes:
• Spondylolisthesis can have various causes, including:
• Congenital (from birth) abnormalities in the spine.
• Degenerative changes in the spine due to aging.
• Traumatic injury or fractures.
• Repetitive stress or overuse of the spine, common in athletes.
• Certain medical conditions, like spondylolysis (a fracture in the vertebra) or osteoporosis.
Symptoms:
• The symptoms of spondylolisthesis can vary in severity and may include:
• Lower back pain that can radiate into the buttocks or legs.
• Muscle tightness or spasms in the lower back.
• Numbness, tingling, or weakness in the legs.
• Difficulty walking or changes in gait.
• Rarely, it can lead to bowel or bladder dysfunction in severe cases.
Physiotherapy Treatment:
• Physiotherapy can be a valuable part of the treatment plan for spondylolisthesis. The goals of physiotherapy include:
• Strengthening the core and back muscles to stabilize the spine.
• Improving flexibility and mobility.
• Reducing pain and discomfort through manual therapy and exercises.
• Teaching proper posture and body mechanics.
• Providing guidance on activity modification and lifestyle adjustments.
Prevention:
• Preventing spondylolisthesis primarily involves reducing risk factors:
• Maintain a healthy weight to minimize stress on the spine.
• Engage in regular physical activity to keep the spine strong and flexible.
• Use proper techniques for lifting and bending to protect the spine.
• If participating in sports, practice good conditioning and follow safety guidelines to prevent injury.
For a comprehensive evaluation, diagnosis, and tailored treatment plan for spondylolisthesis, it's important to consult with a healthcare professional or physiotherapist. They can provide guidance on the most suitable approach for your specific condition and needs.
15. SI Joint dysfunction
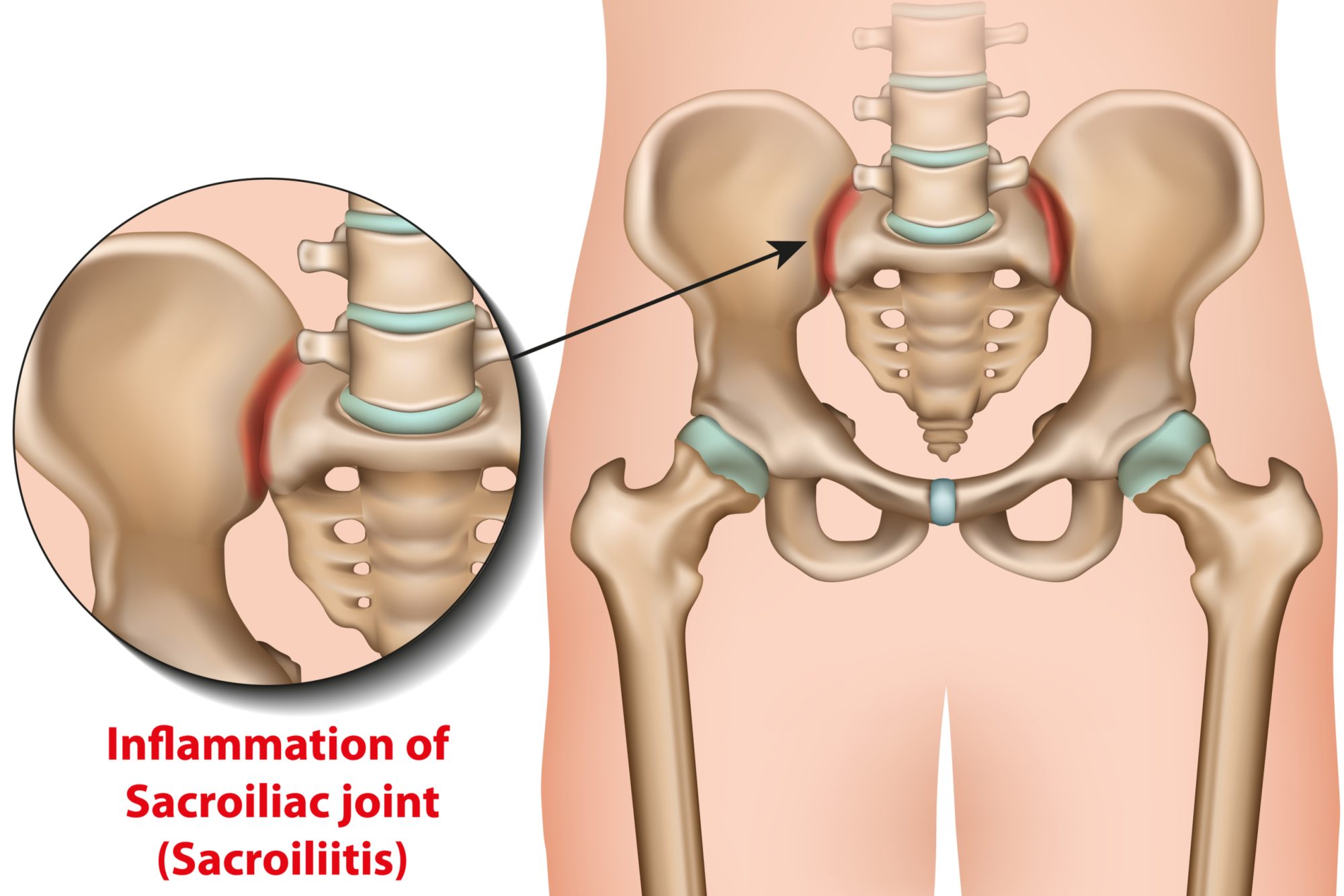
Sacroiliac (SI) joint dysfunction is a condition where the sacrum (the triangular bone at the base of the spine) and the ilium (part of the pelvis) are not functioning properly together. The SI joint plays a crucial role in connecting the spine to the pelvis and transferring forces between the upper body and legs. Dysfunction in this joint can lead to pain and discomfort.
Causes:
• SI joint dysfunction can have various causes, including:
• Arthritis or degeneration of the joint.
• Trauma, such as a fall or injury.
• Pregnancy-related changes.
• Overuse or repetitive stress, common in athletes.
• Muscle imbalances that affect joint stability.
Symptoms:
• Symptoms of SI joint dysfunction may include:
• Pain in the lower back, buttocks, or legs.
• Pain that worsens with sitting, standing, or walking.
• Stiffness or a feeling of the leg "giving way."
• Reduced range of motion in the hip or lower back.
Physiotherapy Treatment:
• Physiotherapy can be effective in managing SI joint dysfunction. Treatment typically includes:
• Manual therapy to mobilize and stabilize the joint.
• Specific exercises to strengthen the muscles supporting the SI joint.
• Stretching to improve flexibility and reduce muscle tension.
• Pain management techniques, such as heat or ice therapy.
• Education on proper posture and body mechanics.
Prevention:
• Reducing the risk of SI joint dysfunction can involve:
• Maintaining a healthy weight to minimize stress on the joint.
• Regularly exercising to keep the supporting muscles strong and flexible.
• Using proper techniques for lifting and bending.
• During pregnancy, using supportive belts or pillows to alleviate pressure on the SI joint.
It's important to consult with a healthcare professional or physiotherapist for an accurate diagnosis and a personalized treatment plan if you suspect SI joint dysfunction. They can provide guidance on the most suitable approach for your specific condition and needs.
16. Sciatica
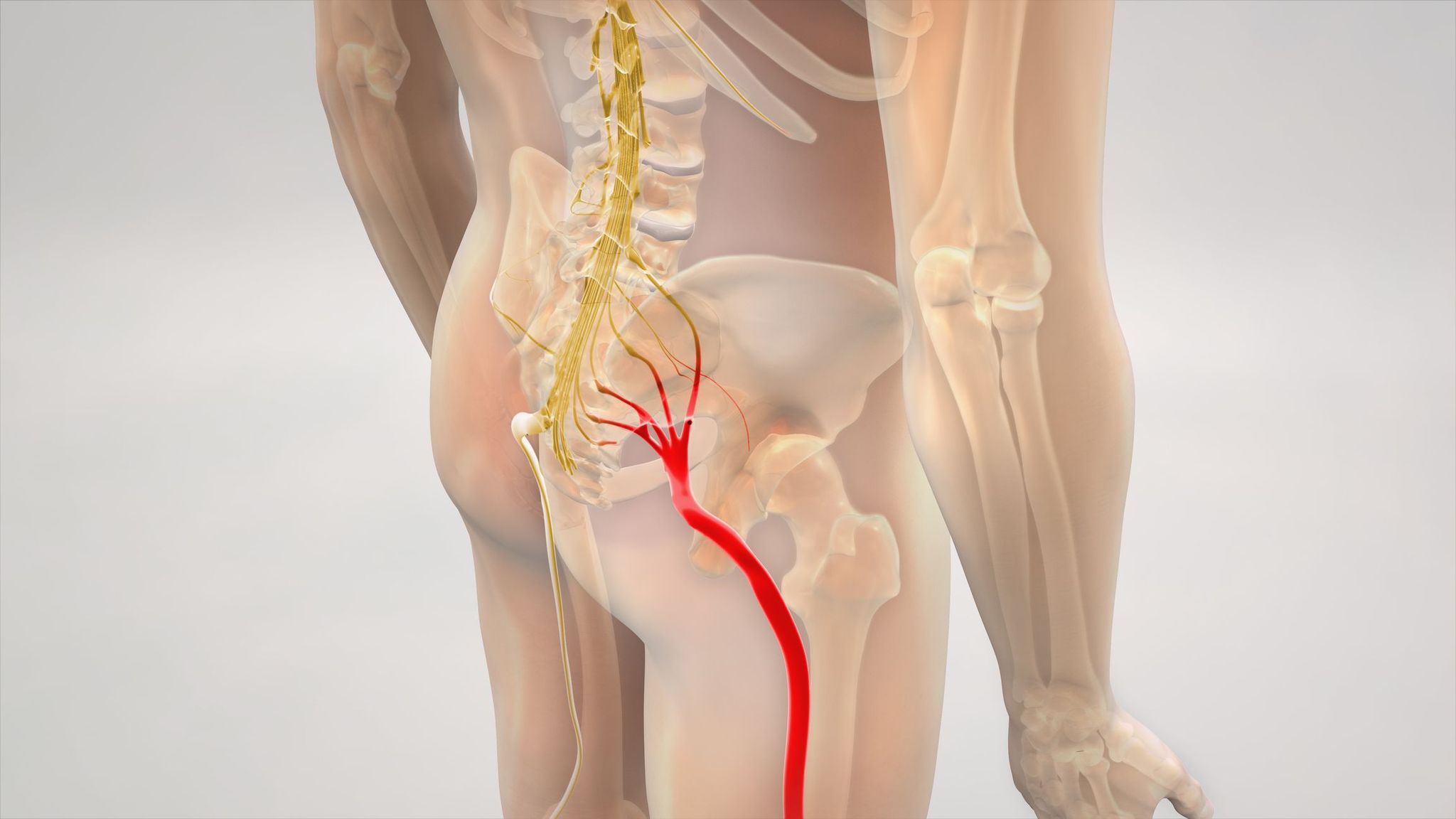
Sciatica is a condition that involves pain, numbness, or tingling that radiates along the sciatic nerve, typically from the lower back down one leg.
Sciatica is not a diagnosis but a set of symptoms caused by irritation or compression of the sciatic nerve, which is one of the largest nerves in the body.
• It can be a result of various underlying conditions and injuries.
Causes:
• Sciatica can be caused by:
• Herniated or slipped discs in the lumbar spine.
• Degenerative disc disease.
• Spinal stenosis (narrowing of the spinal canal).
• Piriformis syndrome (compression of the sciatic nerve by the piriformis muscle).
• Traumatic injuries or fractures.
• Tumors or infections (rarely).
Symptoms:
• Symptoms of sciatica typically include:
• Sharp, shooting pain that radiates from the lower back or buttock down the back of one leg.
• Numbness, tingling, or weakness in the affected leg.
• Pain may worsen with certain movements, such as sitting, standing, or coughing.
Physiotherapy Treatment:
• Physiotherapy is a key component of managing sciatica. Treatment goals include:
• Pain relief through manual therapy techniques.
• Stretching exercises to improve flexibility and relieve nerve compression.
• Strengthening exercises to stabilize the spine and improve posture.
• Postural education to minimize strain on the lower back.
• Advice on ergonomics and proper body mechanics.
Prevention:
• Preventing sciatica involves reducing risk factors and maintaining spine health:
• Regular exercise to strengthen core and back muscles.
• Proper lifting techniques to avoid back injuries.
• Maintaining a healthy weight to reduce strain on the spine.
• Using good posture when sitting or standing for extended periods.
• Engaging in activities that promote spinal flexibility.
If you suspect sciatica or are experiencing symptoms, consult a healthcare professional or physiotherapist for a proper diagnosis and to discuss the most suitable treatment and prevention strategies for your specific condition.
17. Piriformis Syndrome
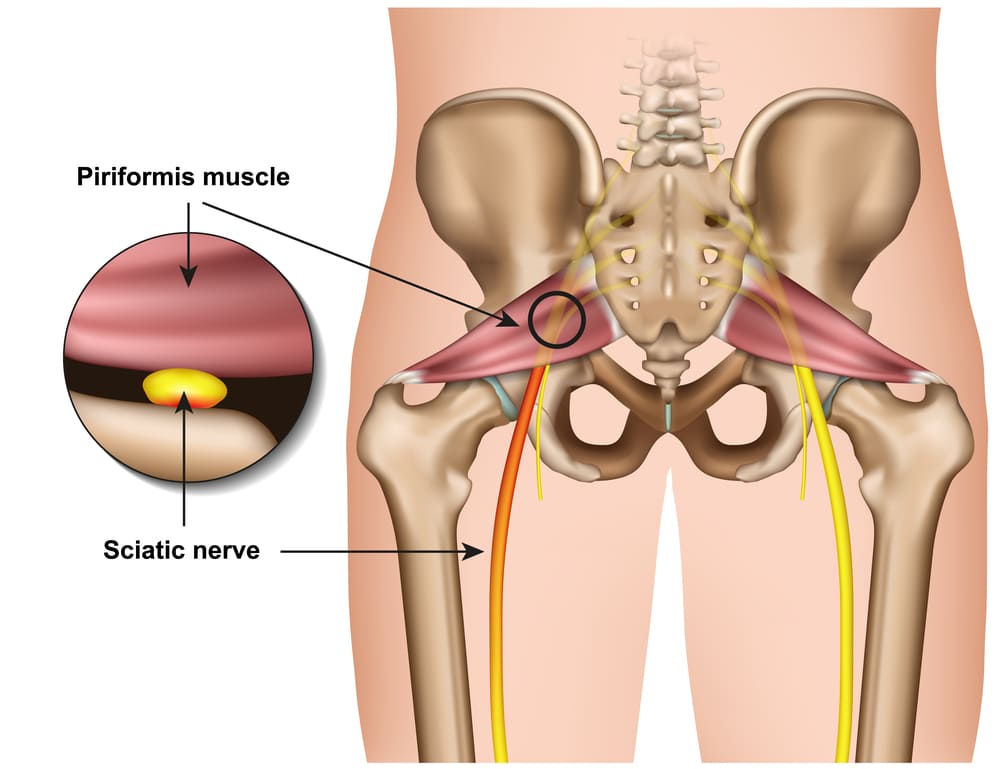
Piriformis syndrome is a condition where the piriformis muscle, located in the buttocks, compresses or irritates the sciatic nerve, leading to pain and discomfort.Piriformis syndrome is a neuromuscular disorder in which the piriformis muscle, situated deep within the buttocks, can put pressure on the sciatic nerve.This compression often results in symptoms similar to sciatica, such as pain, numbness, and tingling in the buttocks and down the leg.
Causes:
• The exact cause of piriformis syndrome is often not clear, but it can be associated with various factors, including:
• Overuse or muscle strain of the piriformis muscle.
• Muscle spasms or tightness in the piriformis.
• Anatomical variations that affect the relationship between the muscle and the nerve.
• Trauma or injury to the buttocks.
Symptoms:
• Common symptoms of piriformis syndrome include:
• Pain in the buttocks that may radiate down the back of the leg.
• Numbness and tingling in the affected leg.
• Difficulty sitting for extended periods.
• Pain that worsens with activities that involve the hip, such as walking or climbing stairs.
Physiotherapy Treatment:
• Physiotherapy plays a crucial role in managing piriformis syndrome. Treatment may include:
• Stretching and flexibility exercises to relieve muscle tension.
• Strengthening exercises for the piriformis and surrounding muscles.
• Manual therapy techniques to alleviate muscle spasms and reduce pain.
• Postural correction and ergonomic advice to avoid exacerbating symptoms.
• Nerve gliding exercises to improve sciatic nerve mobility.
Prevention:
• Reducing the risk of piriformis syndrome and its recurrence involves:
• Maintaining good muscle flexibility through regular stretching.
• Strengthening the muscles in the lower back and pelvis.
• Using proper body mechanics when lifting or performing activities that engage the hip muscles.
• Practicing a balanced exercise routine that includes activities to promote hip and lower back health.
If you suspect piriformis syndrome or are experiencing symptoms, it's important to consult with a healthcare professional or physiotherapist for a proper diagnosis and to discuss the most suitable treatment and prevention strategies for your specific condition.
18. Chondromalacia patella
Chondromalacia patella, also known as "runner's knee," is a condition that affects the cartilage beneath the kneecap. Here's an overview of chondromalacia patella, including its causes, symptoms, physiotherapy, treatment, and prevention:
Introduction: Chondromalacia patella is a condition where the cartilage on the underside of the kneecap softens and deteriorates, leading to pain and discomfort. It often results from overuse, injury, or misalignment of the kneecap.
Causes:
• Overuse or repetitive stress on the knee joint, common in athletes or those with high-impact activities.
• Muscle imbalances around the knee, which can alter the alignment of the kneecap.
• Trauma or injury to the knee joint.
• Arthritis or underlying structural issues.
Symptoms:
• Pain around or under the kneecap, particularly when climbing stairs, kneeling, or sitting for extended periods.
• A grinding or cracking sensation in the knee.
• Swelling or inflammation.
• Weakness or instability in the knee.
Physiotherapy: Physiotherapy plays a crucial role in managing chondromalacia patella. It typically includes:
• Strengthening exercises for the muscles around the knee, especially the quadriceps and hamstrings.
• Stretching exercises to improve flexibility.
• Patellar taping or bracing to provide support and alignment.
• Gait analysis to correct any abnormal walking patterns.
Treatment: Treatment may involve a combination of the following:
• Rest and activity modification to reduce stress on the knee.
• Pain management with ice, anti-inflammatory medications, or injections.
• Physiotherapy, as mentioned above.
• In severe cases, surgery may be required to repair or realign the kneecap or damaged cartilage.
Prevention: To prevent chondromalacia patella:
• Maintain a balanced exercise routine to avoid overuse.
• Use proper form and technique when exercising.
• Wear appropriate footwear for your activities.
• Address muscle imbalances through strength training.
• Warm up and cool down before and after exercise.
• Listen to your body and seek early treatment for any knee pain or discomfort.
It's essential to consult a healthcare professional for a proper diagnosis and personalized treatment plan if you suspect you have chondromalacia patella.
19. Fibromyalgia
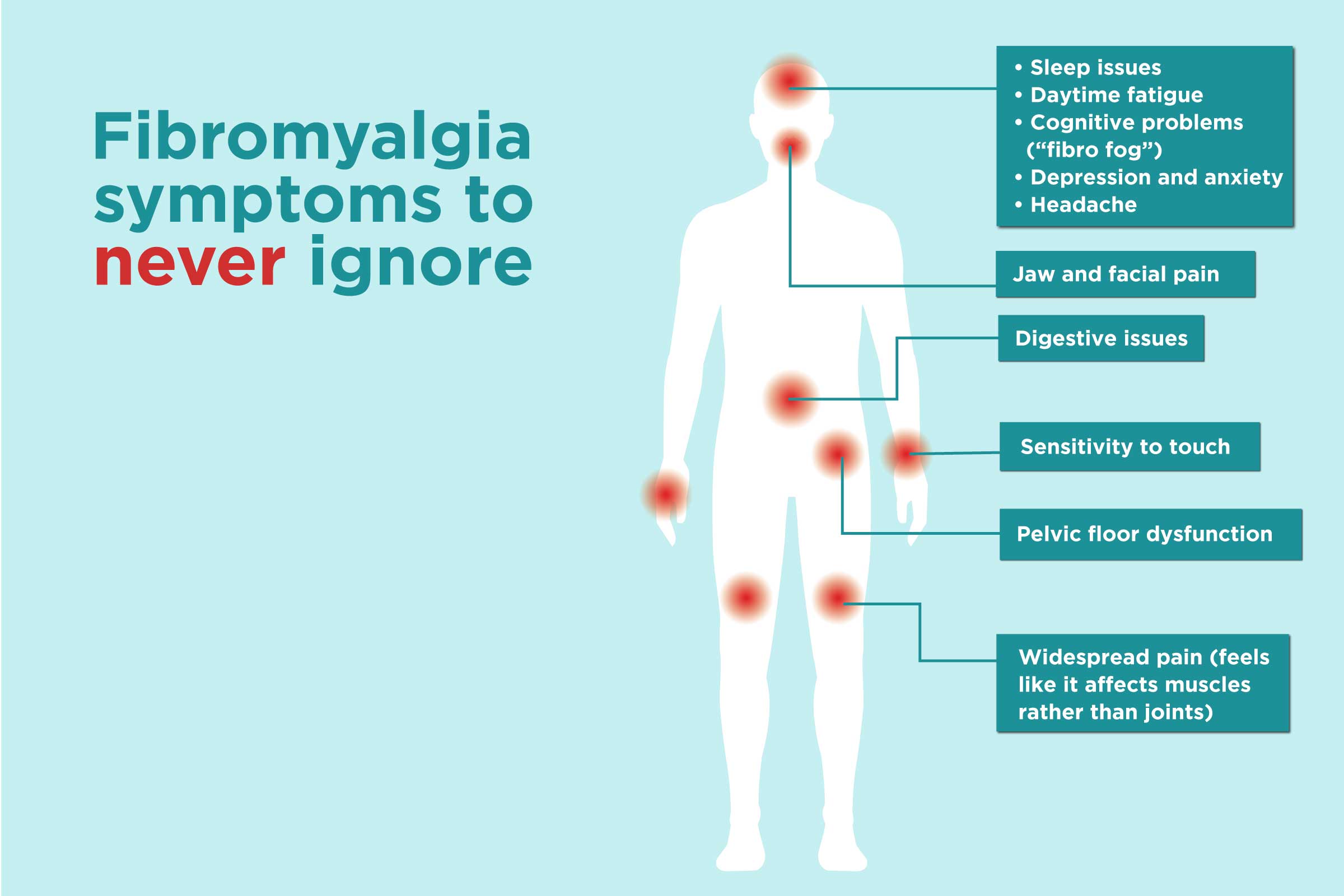
Introduction: Fibromyalgia is a chronic pain disorder characterized by widespread musculoskeletal pain, fatigue, and tenderness in specific points on the body. It is a complex condition that can be challenging to diagnose and manage.
Causes: The exact cause of fibromyalgia is not well understood, but it's believed to involve a combination of genetic, environmental, and neurological factors. Some potential triggers and associations include:
• Genetics - It may run in families.
• Infections or illnesses that initiate or exacerbate symptoms.
• Physical or emotional trauma.
• Abnormal pain processing in the central nervous system.
Symptoms:
• Widespread pain and tenderness in specific trigger points throughout the body.
• Fatigue and sleep disturbances, including non-restorative sleep.
• Cognitive difficulties (often called "fibro fog") that affect memory and concentration.
• Morning stiffness and headaches.
• Irritable bowel syndrome (IBS) and other gastrointestinal issues.
• Sensitivity to temperature, light, and sound.
• Depression and anxiety are commonly associated with fibromyalgia.
Physiotherapy: Physiotherapy can be a valuable part of fibromyalgia management, focusing on:
• Gentle exercise and stretching to improve flexibility and reduce pain.
• Teaching relaxation techniques to manage stress and improve sleep.
• Hydrotherapy (water-based exercises) for pain relief.
• Posture and body mechanics training.
• Education about the condition and self-help strategies.
Treatment: There's no cure for fibromyalgia, but treatment aims to alleviate symptoms and improve the patient's quality of life. Common approaches include:
• Medications for pain, sleep, and mood management.
• Cognitive-behavioral therapy to address emotional and psychological aspects.
• Lifestyle modifications, including regular exercise and stress management.
• Alternative therapies like acupuncture and massage.
• Support groups to connect with others facing similar challenges.
Prevention: Preventing fibromyalgia is difficult due to its unclear causes, but some strategies may help manage the condition or reduce the risk of its onset:
• Maintain a healthy lifestyle with regular exercise and a balanced diet.
• Manage stress through relaxation techniques or mindfulness.
• Ensure good sleep hygiene practices.
• Seek early medical attention for any unexplained or persistent pain.
Fibromyalgia is a chronic condition that often requires ongoing management and a multidisciplinary approach involving healthcare professionals, including rheumatologists, pain specialists, and physiotherapists.
20. Post operation fracture rehabilitation

Introduction: Post-operative fracture rehabilitation is a critical phase of recovery for individuals who have undergone surgery to repair a broken bone. It involves a structured approach to restore strength, mobility, and function to the affected area and facilitate a return to daily activities.
Causes: Fractures occur due to various causes, such as falls, sports injuries, accidents, or underlying medical conditions that weaken the bones. Surgical intervention becomes necessary in cases of severe or complex fractures, joint fractures, or fractures that don't heal properly with conservative treatments.
Symptoms: The symptoms of a fracture depend on the location and severity, but common signs include:
• Pain and swelling at the injury site.
• Deformity or loss of normal alignment.
• Bruising or discoloration.
• Limited or painful movement of the injured limb.
• Numbness or tingling in the area.
• Open wounds or bone protrusion in compound fractures.
Importance: Post-operative fracture rehabilitation is crucial for several reasons:
• Optimal Healing: It promotes proper bone healing and alignment, reducing the risk of complications.
• Restoration of Function: Rehabilitation helps restore strength, mobility, and function to the affected area, allowing the individual to regain independence.
• Pain Management: It aids in managing pain and discomfort during the recovery process.
• Prevention of Complications: It reduces the risk of complications like muscle atrophy, joint stiffness, and blood clots.
• Enhanced Quality of Life: Successful rehabilitation leads to a better quality of life by enabling the individual to return to normal activities.
Physiotherapy: Physiotherapy is a fundamental component of post-operative fracture rehabilitation. It involves:
• Range of Motion Exercises: Gradual and controlled movements to improve joint flexibility.
• Strength Training: Targeted exercises to rebuild muscle strength.
• Functional Training: Activities that mimic daily tasks to enhance practical function.
• Pain Management: Techniques like heat, cold therapy, and manual therapy to alleviate pain and inflammation.
• Education: Teaching proper body mechanics and techniques to prevent future injuries.
Treatment: Treatment post-operation includes:
• Immobilization: In some cases, casts, braces, or splints are used to keep the fracture stable.
• Medications: Pain relievers and anti-inflammatories to manage discomfort and swelling.
• Surgical Hardware: In the case of fractures fixed with screws, plates, or rods, these may need to be removed in a separate procedure once healing is complete.
• Regular Follow-Up: Monitoring progress and adjusting the treatment plan as necessary.
• Activity Modification: Gradually increasing physical activity while avoiding overexertion.
Prevention: Preventing fractures is crucial, and some strategies include:
• Fall Prevention: Especially in the elderly, addressing hazards that can lead to falls.
• Safety Measures: Using protective gear in sports and ensuring a safe environment at work and home.
• Nutrition: Maintaining bone health through a balanced diet rich in calcium and vitamin D.
• Regular Exercise: To build and maintain bone density and muscle strength.
In conclusion, post-operative fracture rehabilitation plays a vital role in ensuring a successful recovery, reducing complications, and restoring a patient's quality of life after a fracture surgery.
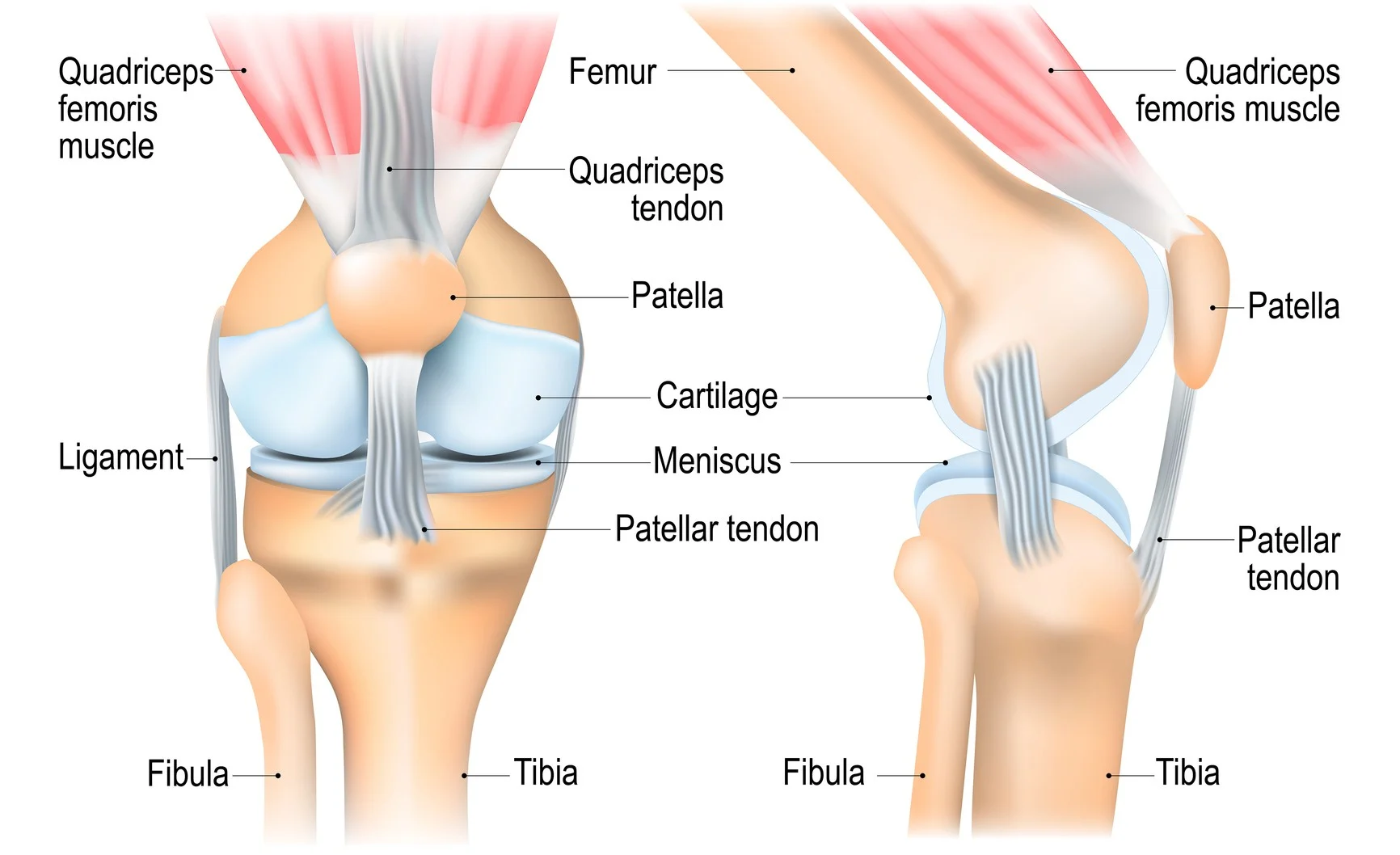
21. TKR (Total knee replacement)
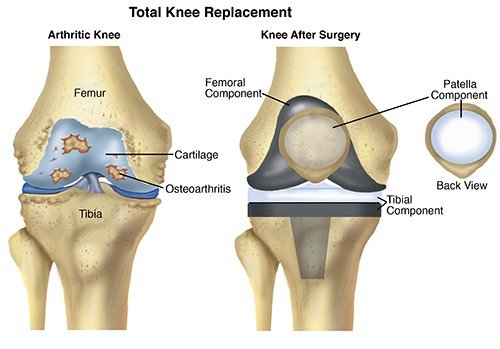
Introduction: Total knee replacement, also known as knee arthroplasty, is a surgical procedure that involves replacing a damaged or worn-out knee joint with an artificial implant. This procedure is performed to relieve pain and improve the function of the knee when other treatments have not been successful.
Causes: Total knee replacement is typically performed due to the following causes:
• Osteoarthritis: The most common reason, as the protective cartilage in the knee joint wears down with age.
• Rheumatoid Arthritis: An autoimmune condition that can damage the knee joint.
• Traumatic Injuries: Severe injuries to the knee joint, such as fractures or ligament tears.
• Other Conditions: Rarely, conditions like avascular necrosis or severe deformities may necessitate a knee replacement.
Symptoms: The symptoms that often lead to considering a total knee replacement include:
• Chronic knee pain that is not relieved by medications or other treatments.
• Significant stiffness in the knee joint, leading to limited range of motion.
• Swelling and inflammation around the knee.
• Difficulty in walking, climbing stairs, or performing daily activities due to knee pain and dysfunction.
Physiotherapy: Physiotherapy is a crucial part of the rehabilitation process following a total knee replacement. It includes:
• Range of Motion Exercises: To improve flexibility and prevent stiffness.
• Strength Training: To rebuild the muscles around the knee joint.
• Gait Training: Teaching proper walking patterns and balance.
• Pain Management: Techniques such as ice, heat, and manual therapy.
• Education: Providing information on post-surgery care and exercises to maintain knee health.
Treatment: The primary treatment for advanced knee joint issues is a total knee replacement, involving:
• Surgical Procedure: The damaged parts of the knee joint are removed, and the artificial implant is secured in place.
• Post-operative Care: Patients are closely monitored in the hospital after surgery and are provided with pain management and physical therapy.
• Rehabilitation: A comprehensive rehabilitation program is crucial to regain knee function.
Prevention: Preventing the need for a total knee replacement can be challenging, but strategies to maintain joint health include:
• Weight Management: Maintaining a healthy weight reduces stress on the knee joints.
• Regular Exercise: Strengthening the muscles around the knee and maintaining flexibility.
• Injury Prevention: Taking precautions to avoid traumatic injuries to the knee.
• Proper Footwear: Wearing shoes that provide good support and cushioning.
• Medical Management: Treating underlying conditions like arthritis to slow down joint deterioration.
Total knee replacement is a highly effective procedure for improving the quality of life for individuals with severe knee joint problems. However, it's typically considered after other conservative treatments have been exhausted, and it's essential to consult with a healthcare professional for an accurate diagnosis and treatment plan.
22. OA
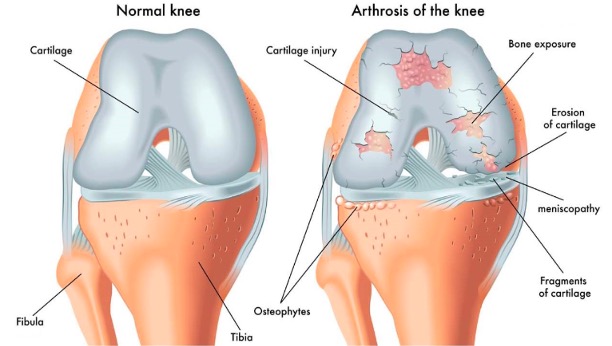
Introduction: Osteoarthritis is a degenerative joint disease that affects the cartilage, which is the protective tissue that covers the ends of bones in a joint. It's the most common form of arthritis and can lead to pain, stiffness, and reduced joint function.
Causes: The exact cause of osteoarthritis is not fully understood, but it's believed to result from a combination of factors, including: • Age: Osteoarthritis becomes more common as people get older.
• Genetics: A family history of the condition can increase the risk.
• Joint Overuse: Repetitive stress or injury to a joint can contribute.
• Obesity: Excess weight puts added stress on weight-bearing joints.
• Joint Misalignment or Injury: Previous joint injuries or congenital joint abnormalities can be a factor.
Symptoms: Symptoms of osteoarthritis include:
• Joint Pain: Often worse with activity and alleviated with rest.
• Stiffness: Especially in the morning or after periods of inactivity.
• Reduced Range of Motion: Joints may not move as freely as they once did.
• Grating Sensation: A feeling or sound of bone rubbing against bone.
• Swelling: Inflammation can occur around the affected joint.
• Bony Enlargements: In some cases, the formation of bony outgrowths (bone spurs).
Physiotherapy: Physiotherapy is a key component of managing osteoarthritis. It focuses on:
• Exercise: Strengthening the muscles around the affected joint to provide better support.
• Range of Motion Exercises: To improve flexibility and reduce stiffness.
• Pain Management: Techniques such as heat or cold therapy, and manual therapy.
• Assistive Devices: Recommending and fitting devices like braces or canes when necessary.
• Education: Teaching patients about the condition and self-management strategies.
Treatment: Treatment for osteoarthritis includes a range of options, which can be tailored to the individual's needs:
• Medications: Pain relievers, anti-inflammatory drugs, and in some cases, injections of corticosteroids or hyaluronic acid.
• Physical and Occupational Therapy: As mentioned earlier, these therapies aim to improve joint function.
• Weight Management: Maintaining a healthy weight can reduce the stress on weight-bearing joints.
• Assistive Devices: Devices like braces or shoe inserts can help support the affected joints.
• Surgical Options: In severe cases, joint replacement surgery may be considered.
Prevention: While osteoarthritis is not always preventable, some strategies can reduce the risk or slow its progression:
• Maintain a Healthy Weight: Obesity is a significant risk factor.
• Exercise Regularly: Strengthening the muscles around joints can provide better support.
• Protect Joints: Avoid overuse and joint injuries, and use proper body mechanics.
• Stay Active: Regular physical activity can help maintain joint health and flexibility.
• Use Joint Protection Techniques: Avoid activities that put excessive stress on joints.
Osteoarthritis is a chronic condition that requires ongoing management. Early diagnosis and a comprehensive approach to treatment and self-care can significantly improve a person's quality of life while living with this condition.
23.Rheumatoid arthritis

Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints. It occurs when the immune system mistakenly attacks healthy joint tissues, leading to inflammation, pain, and joint damage.
Causes: The exact cause of RA is not well understood, but it is believed to result from a combination of genetic and environmental factors. Certain genes may increase susceptibility, and factors like smoking and infections can contribute to the development of RA.
Symptoms:
• Joint pain and swelling, often symmetrical
• Morning stiffness in affected joints
• Fatigue
• Loss of joint function
• Systemic symptoms, like fever and weight loss
Physiotherapy: Physiotherapy plays a crucial role in managing RA by:
• Improving joint mobility and muscle strength.
• Reducing pain and inflammation.
• Enhancing overall physical function.
• Providing guidance on assistive devices.
Treatment: RA treatment focuses on controlling inflammation and managing symptoms. It includes:
• Medications (NSAIDs, DMARDs, biologics)
• Physical therapy
• Lifestyle modifications
• In some cases, surgery to repair or replace damaged joints.
Prevention: RA is not entirely preventable, but you can reduce your risk by:
• Avoiding smoking.
• Maintaining a healthy weight.
• Staying physically active.
• Managing stress.
• Early diagnosis and prompt treatment can help prevent joint damage.
Consult a healthcare professional for a personalized approach to RA management.
24.Golfers elbow
Golfer's Elbow, also known as medial epicondylitis, is a condition that causes pain and inflammation in the tendons of the forearm, near the inner side of the elbow. It's often associated with repetitive hand and wrist motions, similar to those used in golf swings.
Causes: Golfer's Elbow is primarily caused by overuse of the forearm muscles and tendons. Repetitive gripping, twisting, or flexing of the wrist can lead to small tears in the tendons.
Symptoms:
• Pain and tenderness on the inner side of the elbow.
• Weakness in the hand and wrist.
• Stiffness in the elbow.
• Pain when gripping or lifting objects.
• Numbness or tingling in the fingers.
Physiotherapy: Physiotherapy is an essential component of Golfer's Elbow treatment and includes:
• Stretching and strengthening exercises to improve muscle and tendon flexibility and strength.
• Manual therapy techniques to reduce pain and inflammation.
• Ultrasound or other modalities to promote healing.
• Ergonomic advice to prevent re-injury.
Treatment: Treatment for Golfer's Elbow may involve:
• Rest and activity modification to avoid aggravating movements.
• Ice and anti-inflammatory medications to reduce pain and inflammation.
• A counterforce brace to reduce strain on the tendons.
• Corticosteroid injections in severe cases.
• Surgery if conservative treatments fail.
Prevention: To prevent Golfer's Elbow:
• Use proper equipment and technique in sports and activities.
• Warm up before physical activity.
• Strengthen forearm muscles.
• Take breaks during repetitive tasks.
• Avoid excessive force during gripping.
If you suspect Golfer's Elbow, consult a healthcare professional for an accurate diagnosis and appropriate treatment.
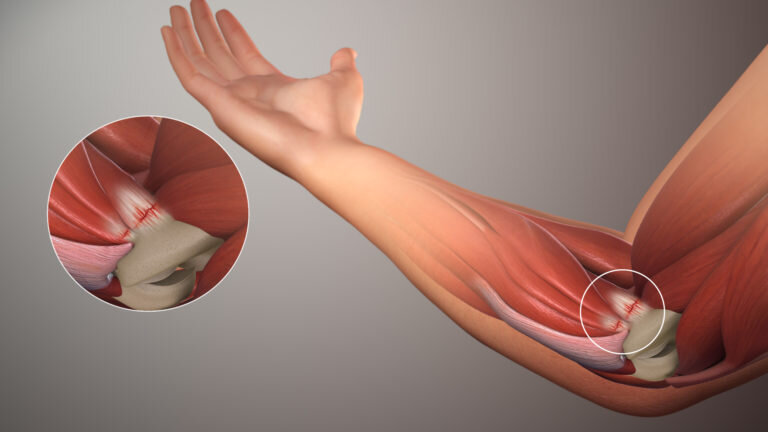
25.Tennjs elbow
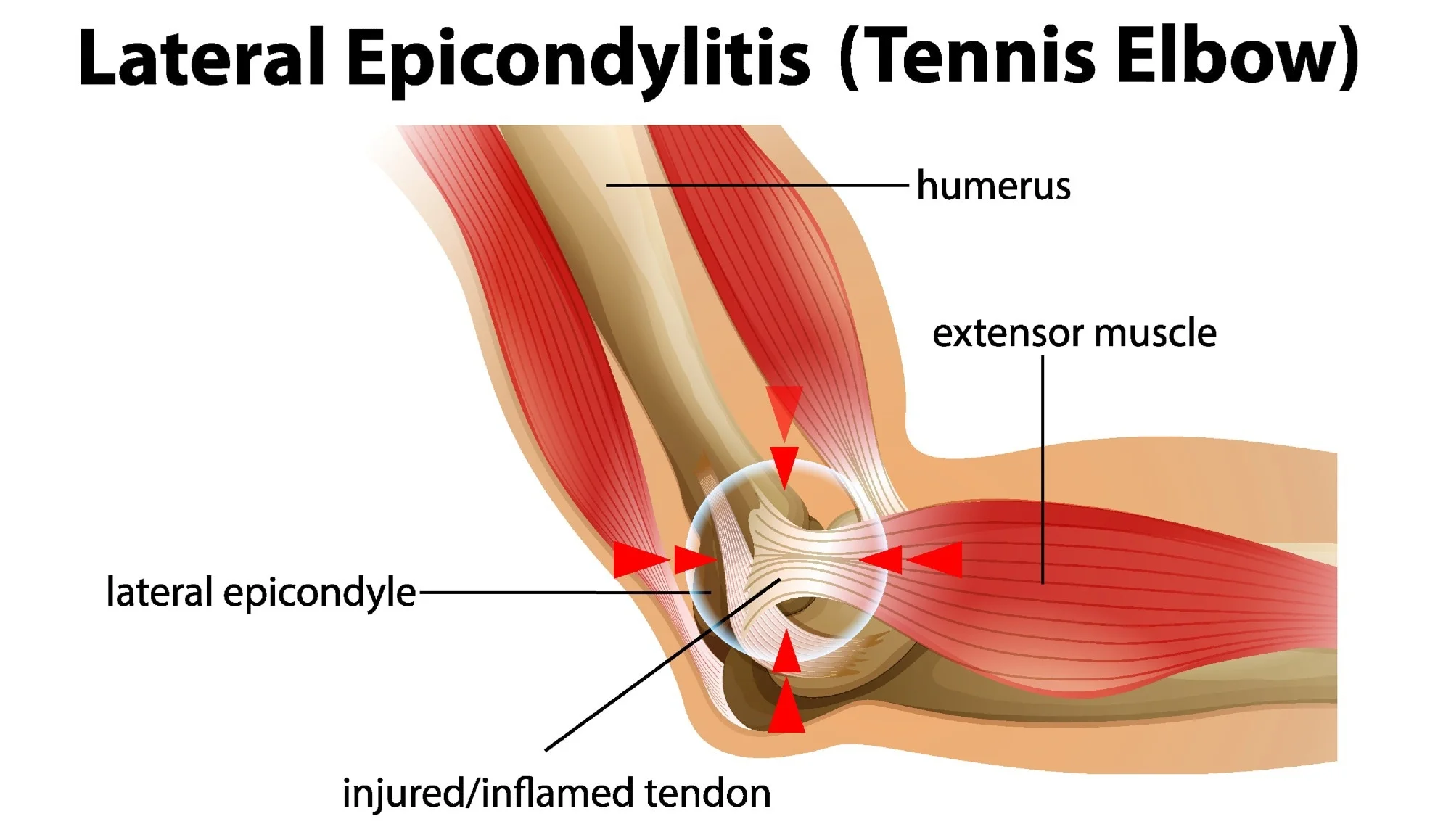
Tennis elbow, also known as lateral epicondylitis, is a condition that affects the tendons in the elbow. It's not limited to tennis players; it can occur in anyone who repetitively uses their forearm muscles. Here's an overview:
Causes:
• Overuse of the forearm muscles, often due to repetitive gripping and wrist extension motions.
• Activities like tennis, typing, or manual labor can lead to this condition.
Symptoms:
• Pain on the outer part of the elbow.
• Weak grip strength.
• Difficulty in activities that involve wrist and hand movements.
Physiotherapy Treatment:
• Rest and avoiding activities that worsen the pain.
• Physical therapy exercises to strengthen and stretch the affected muscles and tendons.
• Modalities like ice, heat, or ultrasound.
• Brace or strap for support.
Prevention:
• Proper technique and equipment use in sports.
• Regular breaks during repetitive tasks.
• Strengthening forearm muscles.
• Stretching exercises.
It's important to consult a healthcare professional for proper diagnosis and treatment tailored to your specific condition.
26.Rotator cuff tear
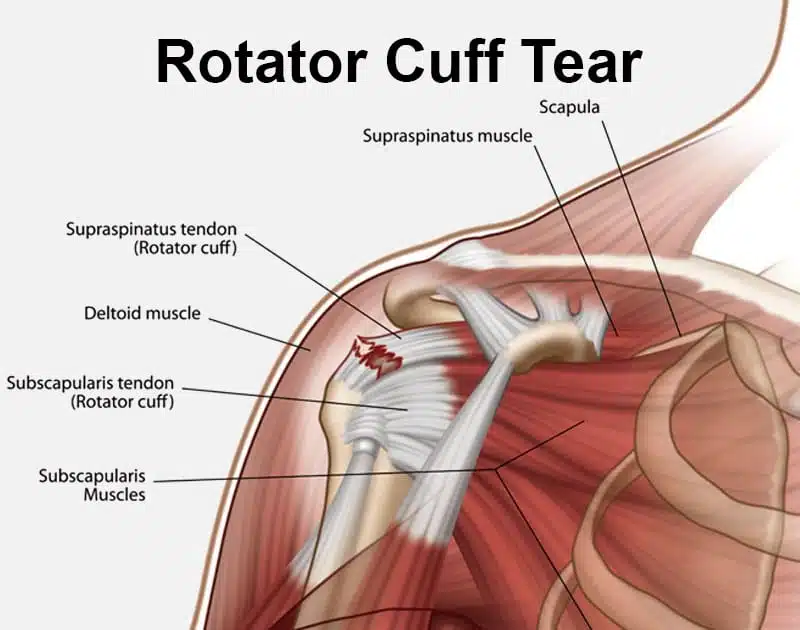
A rotator cuff tear is a common shoulder injury. Here's an overview:
Introduction: The rotator cuff is a group of muscles and tendons that surround the shoulder joint, providing stability and facilitating movement. A rotator cuff tear occurs when one or more of these tendons become damaged or torn.
Causes:
• Aging: As we get older, wear and tear can weaken the tendons.
• Overuse or Repetitive Stress: Activities like lifting, throwing, or sports can strain the rotator cuff.
• Trauma: A fall or direct blow to the shoulder can cause tears.
• Degenerative Changes: Conditions like tendonitis and impingement can weaken the tendons over time.
Symptoms: Common symptoms include pain in the shoulder, especially when lifting or reaching, weakness in the affected arm, and a limited range of motion. You may also experience clicking or popping sensations.
Physiotherapy Treatment: Physiotherapy can be an effective non-surgical approach. It often includes:
• Strengthening exercises: To improve the stability of the shoulder.
• Range of motion exercises: To enhance flexibility.
• Manual therapy: Hands-on techniques to relieve pain and improve function.
• Modalities: Such as heat or ice to manage symptoms.
Prevention: To reduce the risk of a rotator cuff tear:
• Exercise: Strengthen the shoulder muscles.
• Proper Technique: When lifting or playing sports, use correct form.
• Avoid Overuse: Give your shoulder time to rest.
• Posture: Maintain good posture to prevent impingement.
• Warm Up: Always warm up before physical activity.
Severe tears may require surgical intervention, so it's important to consult a healthcare professional for a proper diagnosis and treatment plan.
27.Ligament injury
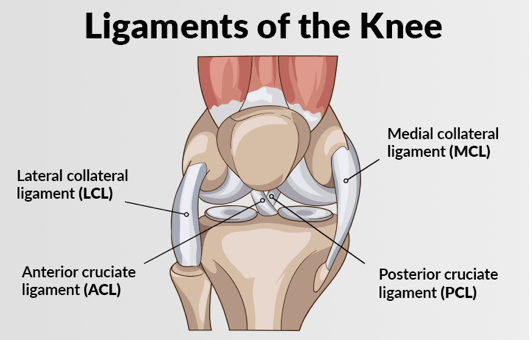
A ligament injury is damage to the tough, fibrous tissues that connect bones and stabilize joints. Here's an overview:
Introduction: Ligaments are crucial for maintaining joint stability and function. Injuries to ligaments can range from mild sprains to severe tears, depending on the extent of damage.
Causes:
• Trauma or Injury: Sudden impacts or twisting motions can strain or tear ligaments.
• Overuse or Repetitive Stress: Continuous stress on a joint, common in athletes, can lead to overuse injuries.
• Aging: Ligaments can become less elastic and more prone to injury with age.
Symptoms: Symptoms of a ligament injury may include pain, swelling, instability in the joint, bruising, and a limited range of motion. Severe injuries can lead to joint dislocation.
Physiotherapy Treatment: Physiotherapy plays a key role in recovering from ligament injuries and often includes:
• RICE Protocol: Rest, ice, compression, and elevation to manage pain and swelling.
• Range of Motion Exercises: Gradual movements to restore joint flexibility.
• Strength Training: Exercises to rebuild muscle support around the injured joint.
• Balance and Proprioception Training: To improve stability and reduce the risk of future injuries.
• Modalities: Such as ultrasound or electrical stimulation for pain relief.
Prevention: To reduce the risk of ligament injuries:
• Proper Warm-Up: Always warm up before exercise to prepare your muscles and ligaments.
• Strength and Flexibility: Maintain good overall strength and flexibility.
• Wear Protective Gear: In contact sports, use appropriate protective equipment.
• Technique: Learn and use correct techniques to prevent overstretching or twisting.
• Rest and Recovery: Allow your body to recover adequately between strenuous activities.
In severe cases, ligament injuries may require surgery, but many can be effectively managed with physiotherapy and conservative treatments. Consulting with a healthcare professional is essential to determine the best course of action for your specific injury.
28.Acl
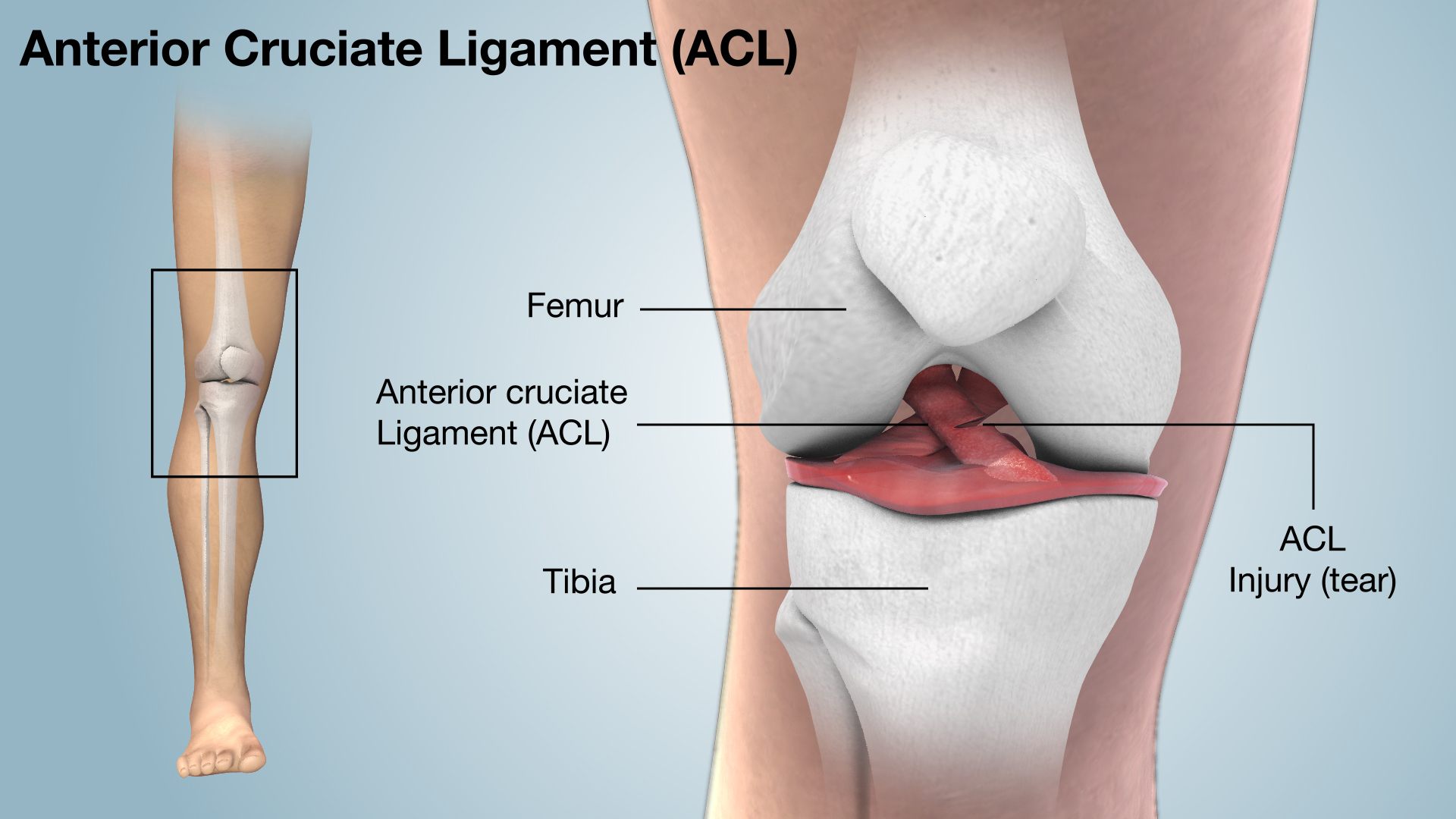
An anterior cruciate ligament (ACL) injury is a common knee injury, particularly in sports. Here's an overview:
Introduction: The ACL is one of the major ligaments in the knee, providing stability and controlling its range of motion. An ACL injury can range from a sprain to a complete tear.
Causes:
• Sudden Stops or Changes in Direction: Common in sports like soccer, basketball, and skiing.
• Direct Impact: A hard blow to the knee.
• Overextension: Hyperextending the knee can lead to injury.
• Non-Contact Injuries: Twisting the knee while pivoting or landing improperly.
Symptoms: Common symptoms of an ACL injury include a popping sound at the time of injury, immediate swelling, severe pain, instability in the knee, difficulty bearing weight, and a limited range of motion.
Physiotherapy Treatment: Physiotherapy is a critical part of ACL injury management and recovery. Treatment typically includes:
• Pre-Surgery Rehabilitation: Strengthening the knee and surrounding muscles before surgical repair.
• Post-Surgery Rehabilitation: After ACL reconstruction, exercises to regain strength and mobility.
• Range of Motion Exercises: To restore knee flexibility.
• Strength Training: Focusing on quadriceps and hamstrings to support the knee.
• Balance and Proprioception Training: Enhancing stability and preventing future injuries.
• Sport-Specific Training: Tailored exercises for return to sports or activities.
Prevention: Preventing ACL injuries can be challenging but here are some strategies:
• Strength Training: Build leg muscles to help support the knee.
• Neuromuscular Training: Programs that improve balance and control.
• Proper Technique: Learn and use proper landing and pivoting techniques.
• Use of Knee Braces: Especially for athletes with a history of ACL injuries.
• Warm-Up and Cool-Down: Always prepare your body for activity and stretch afterward.
Ultimately, if you suspect an ACL injury, it's essential to consult with a healthcare professional for a proper diagnosis and to determine the most appropriate course of treatment, whether that involves surgery or conservative management.
29.PCL
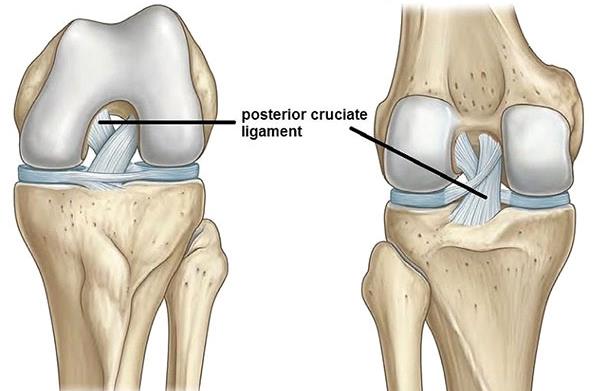
A posterior cruciate ligament (PCL) injury is a less common but still significant knee injury.
Introduction: The PCL is one of the major ligaments in the knee, providing stability by preventing the tibia (shinbone) from moving too far backward in relation to the femur (thighbone). PCL injuries vary in severity and can be classified as sprains or tears.
Causes:
• Direct Impact: Often occurs in motor vehicle accidents or during sports when the knee sustains a blow.
• Hyperextension: Overextending the knee joint, which can stretch or tear the PCL.
• Sports Injuries: Trauma during sports activities, particularly football, soccer, and basketball.
• Falls: A fall onto a bent knee can cause PCL injury.
Symptoms: PCL injury symptoms may include swelling, pain deep within the knee, instability (feeling like the knee will give way), difficulty walking, and a decrease in range of motion.
Physiotherapy Treatment: Physiotherapy is essential for managing PCL injuries and may involve:
• Rest and Protection: Initially, to reduce inflammation and prevent further damage.
• Strengthening Exercises: Focusing on the muscles around the knee to compensate for PCL instability.
• Range of Motion Exercises: To regain flexibility.
• Balance and Proprioception Training: To improve joint stability.
• Modalities: Such as heat, ice, or electrical stimulation to alleviate pain.
Prevention: Preventing PCL injuries can be challenging, but some strategies include:
• Strengthening Exercises: Building strong leg muscles to support the knee.
• Proper Technique: Learning and using correct techniques in sports and activities.
• Protective Gear: Using appropriate safety equipment in high-risk activities.
• Warm-Up and Cool-Down: Preparing the body before activity and stretching afterward.
• Awareness: Be cautious during high-impact situations, such as falls or collisions.
In severe cases of PCL injury, surgery may be necessary, but many can be managed conservatively through physiotherapy and rehabilitation. It's important to consult a healthcare professional to determine the best course of action for your specific injury.
30.Stroke
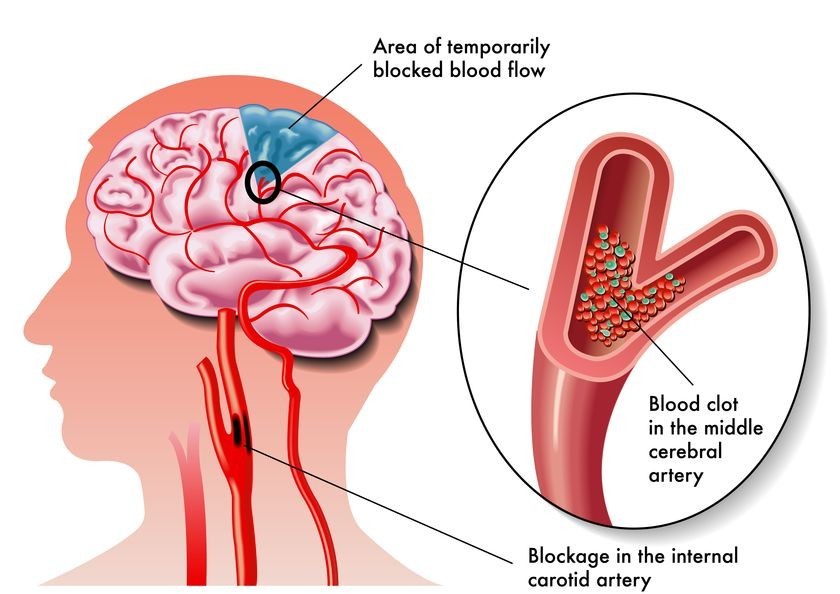
Introduction: A stroke, also known as a cerebrovascular accident (CVA), is a medical emergency that occurs when there is a disruption of blood flow to the brain, leading to brain cell damage. There are different types of strokes, the most common being ischemic and hemorrhagic strokes.
Causes:
• Ischemic Stroke: Caused by a blockage in a blood vessel supplying the brain, often due to a blood clot.
• Hemorrhagic Stroke: Results from the rupture of a blood vessel in the brain, leading to bleeding.
• Transient Ischemic Attack (TIA): Sometimes called a "mini-stroke," it's caused by a temporary blood flow disruption and often a warning sign of an impending stroke.
Symptoms: Symptoms of a stroke can vary but often include sudden:
• Numbness or weakness in the face, arm, or leg, especially on one side of the body.
• Confusion, trouble speaking, or difficulty understanding speech.
• Trouble seeing in one or both eyes.
• Severe headache with no known cause.
• Dizziness, loss of balance, or trouble walking.
Physiotherapy Treatment: Physiotherapy plays a vital role in stroke rehabilitation, addressing various aspects such as:
• Mobility Training: Helping patients regain the ability to walk and move.
• Strength and Coordination Exercises: To improve muscle function.
• Range of Motion Exercises: Maintaining flexibility.
• Functional Activities: Training for daily tasks like dressing and grooming.
• Balance and Gait Training: Reducing the risk of falls.
Prevention: To reduce the risk of stroke, consider these measures:
• Healthy Lifestyle: Maintain a balanced diet, regular exercise, and manage stress.
• Manage Hypertension: Keep blood pressure in check.
• Quit Smoking: Smoking increases stroke risk.
• Limit Alcohol: Excessive alcohol consumption can be a risk factor.
• Manage Diabetes: Keep blood sugar levels under control.
• Regular Health Check-ups: Monitor and manage risk factors with your healthcare provider.
• Medication: If prescribed by a doctor for conditions like atrial fibrillation.
In the case of a stroke, it's crucial to seek immediate medical attention, as early intervention can significantly impact the outcome. Recognizing and responding to the signs and symptoms of a stroke is vital for minimizing its effects
31.Head injury
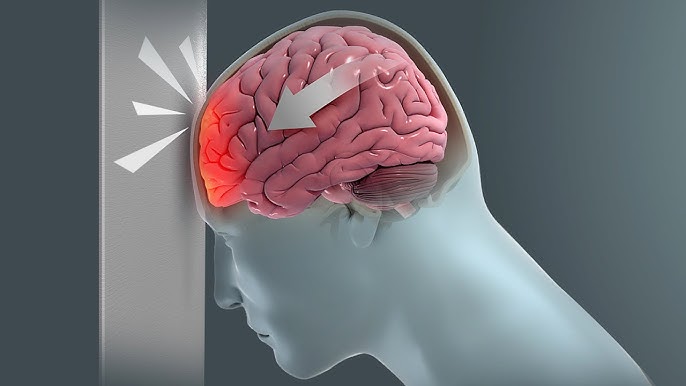
Introduction: A head injury refers to any trauma or damage to the head, scalp, skull, or brain. Head injuries can range from mild concussions to severe traumatic brain injuries (TBIs), and they require prompt evaluation and appropriate treatment.
Causes: Head injuries can result from various causes, including:
• Falls: A common cause, particularly among children and the elderly.
• Motor Vehicle Accidents: Car crashes and accidents involving bicycles or motorcycles.
• Sports Injuries: Concussions or more severe head injuries in contact sports.
• Assaults or Violence: Blows to the head from physical altercations.
• Workplace Accidents: Injuries in occupational settings, especially in construction and industrial jobs.
Symptoms: The symptoms of a head injury can vary depending on the severity but may include:
• Headache
• Dizziness or confusion
• Nausea or vomiting
• Loss of consciousness
• Memory problems
• Changes in behavior or mood
• Difficulty speaking or coordination issues
Physiotherapy Treatment: Physiotherapy can play a role in head injury recovery, particularly in cases where there are associated physical impairments or neurological deficits. Treatment may include:
• Balance and Coordination Exercises: To address issues with mobility and stability.
• Strength and Range of Motion Exercises: To regain muscle function.
• Cognitive Rehabilitation: Techniques to improve memory and cognitive skills.
• Vestibular Rehabilitation: Addressing issues with balance and dizziness.
• Pain Management: Techniques to alleviate headaches or musculoskeletal pain.
Prevention: Preventing head injuries involves taking safety precautions:
• Wear Protective Gear: Helmets for sports, motorcycles, and hard hats in workplaces.
• Seat Belts: Always use seat belts when in a vehicle.
• Fall Prevention: Secure handrails, use non-slip mats, and keep walkways clear.
• Child Safety: Use car seats and childproof homes to prevent falls.
• Violence Prevention: Avoid situations that could lead to head injuries, and seek help if in an abusive situation.
Remember that severe head injuries can be life-threatening, so immediate medical attention is essential in cases of head trauma. For mild head injuries like concussions, it's important to rest and seek medical evaluation if symptoms worsen or persist.
32.Frozen shoulder
Frozen shoulder, also known as adhesive capsulitis, is a condition that affects the shoulder joint, causing stiffness and pain. It typically progresses through several stages, including freezing, frozen, and thawing. Here's an overview of frozen shoulder:
Causes: The exact cause of frozen shoulder is not always clear, but it can be associated with various factors, including:
• Inflammation: Inflammation of the shoulder capsule can lead to the development of scar tissue.
• Immobility: Prolonged immobility of the shoulder due to injury, surgery, or other medical conditions can increase the risk.
• Age and Gender: It's more common in people aged 40 to 60, and it often affects women more than men.
• Medical Conditions: Conditions like diabetes, cardiovascular disease, and thyroid disorders may increase the risk.
Symptoms: Symptoms of frozen shoulder typically progress over time and include:
• Pain: Gradually increasing shoulder pain, especially during movement.
• Stiffness: Limited range of motion, making it difficult to perform daily activities.
• Loss of Function: Decreased strength and function in the affected shoulder.
• Difficulty Sleeping: Pain and discomfort can affect sleep.
Physiotherapy and Treatment: Physiotherapy plays a crucial role in managing frozen shoulder. Treatment options may include:
• Physical Therapy: A physiotherapist can design exercises to improve range of motion and reduce pain.
• Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections can help manage pain and inflammation.
• Heat and Ice Therapy: Applying heat and cold packs can provide relief.
• Home Exercises: A physiotherapist may recommend specific exercises to perform at home.
Prevention: Preventing frozen shoulder may be challenging in cases where it's linked to medical conditions. However, you can reduce the risk by:
• Maintaining Shoulder Health: Regularly perform shoulder exercises to maintain flexibility and strength.
• Managing Medical Conditions: Control conditions like diabetes to lower the risk.
• Early Intervention: If you experience shoulder pain or stiffness, seek medical attention promptly to prevent the condition from worsening.
It's important to consult a healthcare professional for an accurate diagnosis and to determine the most appropriate treatment plan for frozen shoulder.
33.periarthritis

Periarthritis, more commonly known as "periarthritis of the shoulder" or "frozen shoulder," is a condition that affects the shoulder joint, leading to pain and limited mobility. Here's an overview of periarthritis:
Introduction: Periarthritis refers to inflammation and stiffness of the soft tissues surrounding the shoulder joint. It's characterized by pain and restricted movement of the shoulder joint, making everyday activities challenging.
Causes: The exact cause of periarthritis is not always clear, but it can be associated with several factors, including:
• Inflammation: Inflammation of the shoulder capsule and surrounding tissues can contribute to the condition.
• Age and Gender: It's more common in individuals aged 40 to 60 and tends to affect women more than men.
• Immobility: Prolonged immobility of the shoulder due to injury, surgery, or other medical conditions can increase the risk.
Symptoms: Periarthritis of the shoulder typically presents with the following symptoms:
• Shoulder Pain: Gradual onset of pain in the shoulder that may worsen with movement.
• Limited Range of Motion: Decreased ability to move the shoulder joint, resulting in difficulties with daily activities.
• Stiffness: A feeling of stiffness and tightness in the shoulder, especially in the morning.
• Sleep Disturbance: Pain and discomfort can disrupt sleep patterns.
Physiotherapy and Treatment: Physiotherapy is a key component of the treatment plan for periarthritis. Treatment options may include:
• Physical Therapy: A physiotherapist designs exercises to improve range of motion and reduce pain.
• Heat and Ice Therapy: Applying heat and cold packs can help alleviate pain and inflammation.
• Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections may be prescribed to manage pain and inflammation.
• Joint Distension: In some cases, a doctor may use joint distension to stretch the shoulder joint capsule.
• Home Exercises: Patients are often given exercises to perform at home to maintain and improve shoulder function.
Prevention: Preventing periarthritis may be challenging, especially if it's related to underlying medical conditions. However, you can take the following steps to reduce the risk:
• Maintain Shoulder Health: Regularly perform shoulder exercises to maintain flexibility and strength.
• Manage Medical Conditions: Control conditions like diabetes or cardiovascular disease that can increase the risk.
• Early Intervention: Seek medical attention if you experience shoulder pain or stiffness to prevent the condition from worsening.
Consult a healthcare professional for an accurate diagnosis and to determine the most appropriate treatment plan for periarthritis.
34.postural correction

Introduction: Postural correction refers to the process of improving and maintaining proper alignment and positioning of the body when standing, sitting, or during various activities. Good posture is essential for overall musculoskeletal health and can help prevent a range of issues related to poor posture.
Causes: Poor posture can result from various factors, including:
• Habit: Long-standing habits of slouching, hunching over, or poor body mechanics.
• Sedentary Lifestyle: Spending extended periods sitting, especially with inadequate ergonomic support, can contribute to poor posture.
• Muscle Imbalances: Weak or tight muscles can affect posture.
• Medical Conditions: Conditions such as scoliosis or injury can impact posture.
Symptoms: The symptoms of poor posture can vary and may include:
• Musculoskeletal Pain: Back, neck, and shoulder pain are common complaints.
• Fatigue: Poor posture can lead to muscle fatigue and decreased energy.
• Limited Range of Motion: Reduced flexibility and mobility.
• Headaches: Tension headaches can result from neck and shoulder strain.
• Digestive Issues: Poor posture can compress the digestive organs and lead to discomfort.
Physiotherapy and Treatment: Physiotherapy plays a significant role in postural correction. Treatment options may include:
• Postural Education: A physiotherapist can educate individuals about proper posture and ergonomics in various settings.
• Stretching and Strengthening Exercises: Specific exercises can help address muscle imbalances and improve posture.
• Manual Therapy: Hands-on techniques like massage or joint mobilization can be used to relieve muscle tension and pain.
• Modalities: Heat, ice, or electrical modalities may be used to manage pain and inflammation.
• Bracing or Taping: In some cases, bracing or taping can help support and maintain correct posture.
Prevention: Preventing poor posture involves the following strategies:
• Ergonomics: Ensure proper ergonomics in work and home environments, including an ergonomic chair and desk setup.
• Regular Movement: Take breaks to stretch and move, especially if you have a sedentary job.
• Exercise: Maintain overall strength and flexibility through regular physical activity.
• Postural Awareness: Pay attention to your posture throughout the day and make adjustments as needed.
• Ergonomic Furniture: Invest in ergonomic furniture and accessories that support good posture.
Improving and maintaining good posture is essential for long-term musculoskeletal health. Consult a physiotherapist or healthcare professional for personalized guidance on postural correction and related issue.
35.Scoliosis
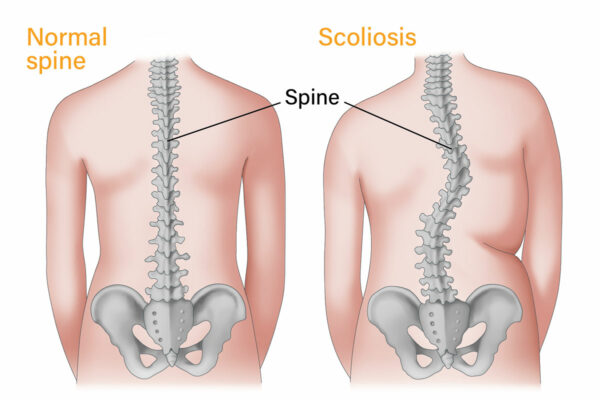
Introduction: Scoliosis is a medical condition characterized by an abnormal lateral curvature of the spine. In a healthy spine, it should have gentle curves when viewed from the side, but scoliosis causes the spine to curve sideways, often in an "S" or "C" shape. This condition can affect people of all ages and can vary in severity.
Causes: The exact cause of scoliosis can be diverse, and it often falls into these categories:
• Idiopathic Scoliosis: This is the most common form, and its cause is unknown. It often develops during adolescence.
• Congenital Scoliosis: Caused by spinal abnormalities present at birth.
• Neuromuscular Scoliosis: Associated with conditions such as cerebral palsy or muscular dystrophy.
• Degenerative Scoliosis: Linked to wear and tear on the spine as a person ages.
Symptoms: The symptoms of scoliosis can vary based on the degree of curvature, but they may include:
• Visible Spinal Curve: Uneven shoulders, hips, or a noticeable curve in the spine when viewed from behind.
• Back Pain: Discomfort or pain, particularly in the lower back.
• Muscle Imbalance: Muscle weakness or tightness on one side of the body.
• Limited Mobility: Reduced range of motion and flexibility.
• Breathing Difficulties: In severe cases, large spinal curves can affect lung function.
Physiotherapy and Treatment: Physiotherapy can be an important part of managing scoliosis, especially for mild to moderate cases. Treatment options may include:
• Postural Education: Physiotherapists teach proper body mechanics and provide guidance on maintaining good posture.
• Exercises: Specific exercises can help improve muscle strength, flexibility, and posture to minimize the progression of the curvature.
• Bracing: In some cases, especially for adolescents with moderate curves, bracing may be recommended to prevent further progression.
• Pain Management: Physiotherapists can help manage pain and discomfort through various techniques.
• Monitoring and Support: Regular check-ups and support to monitor the condition's progress.
Prevention: Preventing scoliosis is challenging, as some forms are congenital or idiopathic. However, early detection and intervention can help prevent the progression of the condition. If scoliosis is diagnosed in a child, timely treatment and physiotherapy can be essential to reduce the severity of the curvature and improve quality of life.
If you suspect scoliosis or have concerns about your spine's alignment, it's crucial to consult a healthcare professional for a thorough evaluation and personalized guidance on treatment and management.
36.Kyphosis
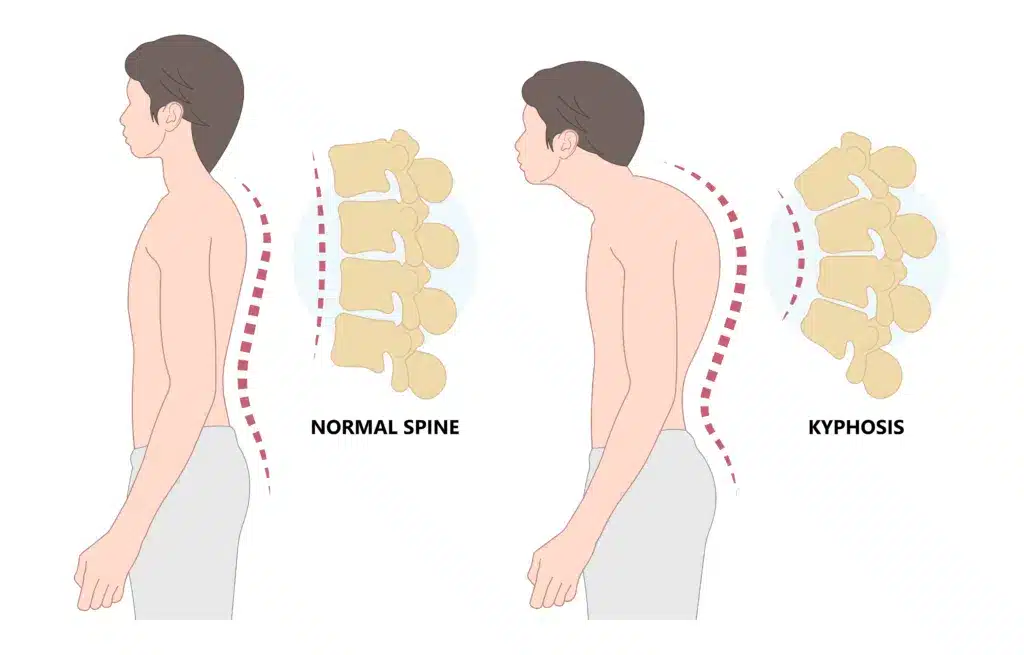
Introduction: Kyphosis is a medical condition characterized by an abnormal forward curvature of the upper spine, leading to a hunched or rounded back. It's often described as "hunchback" or "round back." Kyphosis can affect people of all ages and can vary in severity.
Causes: Kyphosis can have various causes, including:
• Postural Kyphosis: This is often seen in adolescents and is related to poor posture, typically correctable with proper body mechanics and exercises.
• Scheuermann's Kyphosis: This condition typically develops during adolescence and is characterized by structural changes in the vertebrae.
• Congenital Kyphosis: Present at birth, this type is associated with abnormalities in the spine's development.
• Degenerative Kyphosis: Often seen in older adults, this condition results from age-related changes in the spine, such as vertebral compression fractures.
Symptoms: The symptoms of kyphosis can vary based on the degree of curvature, but they may include:
• Visible Round Back: A noticeable curve in the upper spine, leading to a hunched appearance.
• Back Pain: Discomfort or pain, particularly in the upper back.
• Stiffness: Reduced flexibility and range of motion in the spine.
• Muscle Weakness: Weakening of the muscles that support the spine.
• Breathing Difficulties: In severe cases, large spinal curves can affect lung function.
Physiotherapy and Treatment: Physiotherapy can play a vital role in managing and treating kyphosis, depending on the type and severity of the condition. Treatment options may include:
• Postural Education: Physiotherapists teach proper body mechanics and provide guidance on maintaining good posture.
• Exercises: Specific exercises can help improve muscle strength, flexibility, and posture to reduce the severity of the curvature.
• Pain Management: Physiotherapists can help manage pain and discomfort through various techniques.
• Bracing: In some cases, bracing may be recommended for adolescents with significant curves to prevent further progression.
• Surgery: Severe cases of kyphosis may require surgical intervention to correct the curvature.
Prevention: Preventing kyphosis may not always be possible, especially in cases related to congenital or degenerative factors. However, you can reduce the risk of developing postural kyphosis through:
• Postural Awareness: Pay attention to your posture, especially during prolonged periods of sitting or computer use.
• Regular Exercise: Engage in exercises that promote core strength and spinal flexibility.
• Proper Ergonomics: Ensure ergonomic work and home environments to support good posture.
If you suspect kyphosis or have concerns about your spine's alignment, it's essential to consult a healthcare professional for a thorough evaluation and personalized guidance on treatment and management.
37.Lordosis
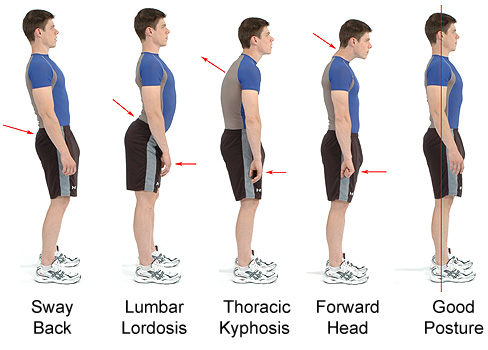
Introduction: Lordosis is a medical condition characterized by an excessive inward curvature of the spine, typically in the lower back (lumbar) or neck (cervical) regions. This exaggerated curve can lead to a "swayback" appearance. Lordosis can affect people of all ages and can vary in severity.
Causes: The causes of lordosis can be diverse, including:
• Postural Lordosis: This is often related to poor posture and can be reversible with proper body mechanics and exercises.
• Spondylolisthesis: A condition where one vertebra slips forward over another, leading to an increased lumbar curve.
• Obesity: Excess weight can affect the spine's alignment and lead to lordotic curvature.
• Muscle Weakness: Weakness in the abdominal or lower back muscles can contribute to lordosis.
• Pregnancy: The increased weight and changes in posture during pregnancy can lead to temporary lordosis.
Symptoms: The symptoms of lordosis can vary based on the degree of curvature, but they may include:
• Exaggerated Curve: A pronounced inward curve in the lower back or neck.
• Back Pain: Discomfort or pain, particularly in the lower back.
• Muscle Weakness: Weakening of the muscles that support the spine.
• Stiffness: Reduced flexibility and range of motion.
• Neurological Symptoms: In severe cases, lordosis can compress spinal nerves, leading to symptoms like tingling, numbness, or weakness in the legs or arms.
Physiotherapy and Treatment: Physiotherapy can be an essential part of managing and treating lordosis, depending on the type and severity of the condition. Treatment options may include:
• Postural Education: Physiotherapists teach proper body mechanics and provide guidance on maintaining good posture.
• Exercises: Specific exercises can help improve muscle strength, flexibility, and posture to reduce the severity of the curvature.
• Pain Management: Physiotherapists can help manage pain and discomfort through various techniques.
• Bracing: In some cases, bracing may be recommended to support the spine and minimize the curvature.
Prevention: Preventing lordosis, particularly postural lordosis, involves the following strategies:
• Postural Awareness: Pay attention to your posture, especially during activities like sitting, standing, or lifting.
• Regular Exercise: Engage in exercises that strengthen the core, abdominal, and lower back muscles to support spinal alignment.
• Weight Management: Maintain a healthy weight to reduce the risk of developing lordotic curvature.
If you suspect lordosis or have concerns about your spine's alignment, it's essential to consult a healthcare professional for a thorough evaluation and personalized guidance on treatment and management.
38.Geriartic care

Geriatric care is a branch of healthcare focused on the unique needs of older adults, typically aged 65 and above. As people age, they may face various physical and mental health challenges. Here's an introduction to geriatric care, including its causes, symptoms, physiotherapy, treatment, and prevention:
Causes of Geriatric Health Issues:
• Aging Process: The natural aging process leads to changes in the body's systems, making older adults more susceptible to health problems.
• Chronic Conditions: Conditions like heart disease, diabetes, and arthritis become more prevalent with age.
• Medication Side Effects: Older adults often take multiple medications, which can have side effects and interactions.
• Lifestyle Factors: Poor nutrition, lack of exercise, and social isolation can contribute to health issues.
Common Symptoms:
• Mobility Issues: Reduced balance, muscle strength, and joint flexibility can lead to falls and fractures.
• Cognitive Decline: Memory problems and cognitive decline may occur.
• Chronic Pain: Conditions like osteoarthritis can cause persistent pain.
• Depression and Isolation: Loneliness and depression are common among older adults.
• Incontinence: Bladder and bowel control may become problematic.
Physiotherapy in Geriatric Care: Physiotherapy plays a crucial role in geriatric care by improving mobility and reducing pain. It includes exercises, manual therapy, and education to enhance strength, balance, and flexibility. This can prevent falls and enhance overall well-being.
Treatment and Management: Treatment in geriatric care is personalized based on the individual's specific health conditions. It may involve medication management, physical therapy, counseling, and lifestyle modifications to address issues like nutrition and social support.
Prevention: • Regular Check-ups: Routine medical check-ups can detect and address health issues early.
• Exercise: Regular physical activity can maintain strength and flexibility.
• Balanced Diet: A healthy diet is essential for overall well-being.
• Medication Management: Reviewing medications with healthcare professionals can prevent adverse interactions.
• Social Engagement: Staying socially active reduces the risk of depression and isolation.
Geriatric care is essential to ensure the quality of life for older adults. It focuses on maintaining independence, managing health issues, and enhancing overall well-being in the aging population.
39.Peadiatric care

Pediatric care is a specialized branch of healthcare focused on the well-being of infants, children, and adolescents. It encompasses a wide range of medical conditions and concerns, with a primary focus on promoting their physical and emotional health. Here's an overview:
Causes: Pediatric conditions can be caused by various factors, including genetic, environmental, infectious, or developmental issues. Common causes include genetic predisposition, infections, injuries, and exposure to toxins.
Symptoms: Symptoms in pediatric care can vary greatly depending on the condition. They may include fever, cough, rash, pain, developmental delays, behavioral changes, and more. The specific symptoms depend on the underlying issue.
Physiotherapy: Physiotherapy is often used in pediatric care to address physical problems. It can help children with mobility issues, developmental delays, or injuries. Pediatric physiotherapists work to improve a child's strength, flexibility, and motor skills.
Treatment: Treatment in pediatric care is tailored to the individual child's needs. It may involve medications, surgery, therapies (e.g., physical, occupational, speech therapy), and counseling. The goal is to alleviate symptoms and support healthy development.
Prevention: Preventive measures in pediatric care include routine vaccinations, proper nutrition, childproofing the home to prevent accidents, regular check-ups, and educating parents and caregivers about child safety and health.
It's important to consult with pediatric healthcare professionals to address specific concerns and get appropriate guidance for your child's care.
40.Sports injury

Introduction: Sports injuries are common occurrences in the world of athletics and physical activities. They can range from minor sprains and strains to more severe injuries such as fractures or torn ligaments. Understanding the causes, symptoms, and treatment options for sports injuries is crucial for both athletes and anyone engaged in physical activities.
Causes: Sports injuries can be caused by various factors, including:
• Trauma: Direct impact or collision with another player or object.
• Overuse: Repeated stress on a specific body part, leading to microtrauma.
• Poor Technique: Incorrect form or posture during sports activities.
• Inadequate Warm-up: Failing to prepare the body properly before physical exertion.
Symptoms: Common symptoms of sports injuries include pain, swelling, bruising, limited range of motion, and difficulty bearing weight. The specific symptoms can vary depending on the type and severity of the injury.
Physiotherapy Treatment: Physiotherapy plays a vital role in the rehabilitation of sports injuries. The treatment may include:
• Assessment: A thorough examination of the injury and its impact on the patient's functional abilities.
• Pain Management: Through techniques such as ice or heat therapy, ultrasound, or electrical stimulation.
• Rehabilitation Exercises: Customized exercise programs to restore strength, flexibility, and range of motion.
• Manual Therapy: Hands-on techniques to improve joint and muscle function.
• Education: Teaching athletes how to prevent future injuries through proper technique and training.
Role of Physiotherapy: Physiotherapy is essential in sports injury management as it:
• Aims to expedite the recovery process, allowing athletes to return to their activities sooner.
• Minimizes the risk of secondary injuries that can occur due to compensatory movements.
• Provides guidance on injury prevention and conditioning.
Prevention: To reduce the risk of sports injuries, individuals should:
• Warm up and stretch properly before engaging in physical activities.
• Use appropriate protective gear and equipment.
• Maintain good physical fitness and conditioning.
• Ensure proper technique and form.
• Listen to their bodies and seek timely medical attention for any discomfort or pain.
In conclusion, sports injuries are common, but with the right approach to prevention and timely physiotherapy treatment, individuals can recover and continue to participate in sports and physical activities safely.
41.Fitness training

Introduction: Fitness training is a crucial aspect of maintaining physical health and overall well-being. It encompasses various exercises and activities designed to improve strength, endurance, flexibility, and cardiovascular health. However, like any physical endeavor, fitness training can sometimes lead to injuries and discomfort. Understanding the causes, symptoms, and the role of physiotherapy in fitness training is essential for a safe and effective training regimen.
Causes: Injuries during fitness training can occur due to several factors, including:
• Overtraining: Pushing the body too hard without adequate rest and recovery.
• Poor Technique: Incorrect form during exercises, which can lead to muscle imbalances or strain.
• Inadequate Warm-up or Cool-down: Skipping warm-up exercises or neglecting to stretch after a workout.
• Muscle Imbalances: Uneven development of muscle groups can lead to overuse injuries.
Symptoms: Symptoms of fitness training-related injuries may include pain, swelling, muscle soreness, limited range of motion, and in some cases, more severe symptoms like muscle tears or joint problems.
Physiotherapy Treatment: Physiotherapy plays a significant role in managing and rehabilitating injuries related to fitness training. Treatment may involve:
• Assessment: A thorough evaluation of the injury and its impact on the patient's ability to exercise.
• Pain Management: Using techniques like ice or heat therapy, manual therapy, or electrical stimulation to reduce pain.
• Rehabilitation Exercises: Customized exercise programs to restore strength, flexibility, and function.
• Manual Therapy: Hands-on techniques to improve joint and muscle function.
• Education: Teaching proper exercise techniques and body mechanics to prevent future injuries.
Role of Physiotherapy: Physiotherapy is essential in fitness training because it:
• Aids in the prompt recovery from injuries, allowing individuals to resume their training.
• Addresses the root causes of injuries, helping to prevent them from recurring.
• Promotes long-term physical health and fitness by providing guidance on safe and effective exercise techniques.
Prevention: To prevent injuries during fitness training, individuals should:
• Gradually increase the intensity of their workouts to avoid overuse injuries.
• Focus on proper form and technique, even if it means lifting lighter weights or doing fewer repetitions.
• Incorporate adequate warm-up and cool-down routines into their training sessions.
• Listen to their bodies and rest when needed to prevent overtraining.
• Seek guidance from fitness professionals or physiotherapists to design a well-balanced workout program.
In conclusion, fitness training is a valuable component of a healthy lifestyle, but injuries can occur if not approached with caution. Physiotherapy is crucial for both treating injuries and promoting safe and effective training practices. Prevention and proper technique are key to a successful and injury-free fitness training regimen.

